Acute Myocardial Infarction in Patients Below 50 Years of Age
M3 India Newsdesk Aug 19, 2024
This article examines acute myocardial infarction (AMI) in patients aged 18-50, focusing on clinical features, coronary involvement, and risk factors.
Case study
To study the clinical features and risk factors among patients of Acute Myocardial Infarction of less than 50 years of age (18-50 years of age) at tertiary care hospitals of Ahmedabad city, Gujarat.
Introduction
Coronary heart disease (CHD) is the leading cause of death in Western countries as well as in India, it has emerged as the top killer that has affected both urban and rural populations. Nonetheless, CAD appeared in India nearly ten years before it did in the West. People over 50 are more likely to develop coronary artery disease (CAD).
Acute myocardial infarction (AMI) among young is relatively uncommon. Still, it is an important problem for the patient and the treating physician, as these patients can have different risk factors, clinical presentation and prognosis than the older patients as follows:
- Smoking
- Obesity
- Hyperlipidaemia
- Family history of premature CHD
- Drug abuse
- Male gender
Patients suffering from AMI at a younger age are reported to have higher body mass index (BMI) and more central obesity. compared to age and gender-matched controls. A high rate of lifetime history of depression and depressive symptoms at the time of an AMI was observed in young AMI patients.
Looking at the paucity of studies on AMI among the young and the increasing trend of AMI among young adults, we proposed this study. The evidence generated by the study on clinical presentation and risk factors of AMI of young may help in designing health education material to create awareness among the young.
Discussion
- The study was conducted on AMI patients of <50 years of age from government and private tertiary care hospitals. A total of 96 patients were studied for their clinical features, coronary involvement and risk factors.
- The mean age of study subjects was 42.08 with an SD of 5.71 years with the minimum age being 27 years. More than 80% of the patients with AMI were>35 years in the present study (Table 1).
- In a retrospective study done in Jharkhand, 52.2% were in the age >35 years. Very few patients are in the age group below 35 years. Most of the patients (88.5%) were males. (figure 1) Male preponderance was found in other studies also,[10],[14],[15],[22].
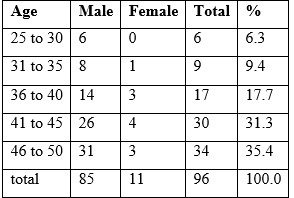
Table 1 Age and sex-wise distribution of study subjects (n=96)
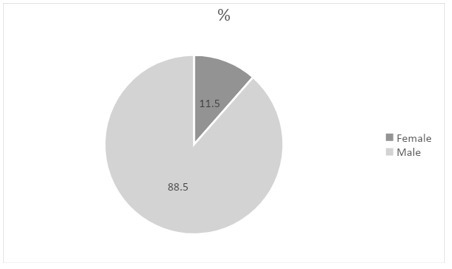
Figure 1 sex wise distribution of study subjects (n=96)
- The female gender generally is protected by the cardioprotective effects of oestrogen until menopause which is usually after the age of 45 years, which may be the reason behind male dominance.
- Two-thirds of patients were working as either skilled workers or in the professional sector or running a business which reflects stressful work life for these patients. Rest were involved in semi-skilled/unskilled work or not working. The majority of the patients belonged to SE class 1 of modified Prasad's classification. (table 2)
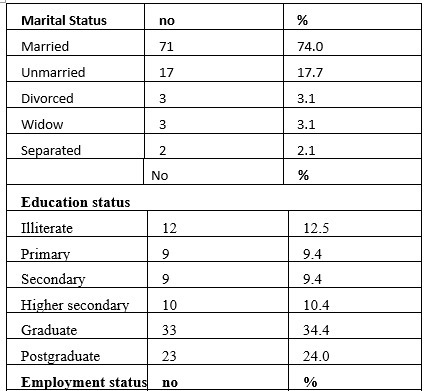
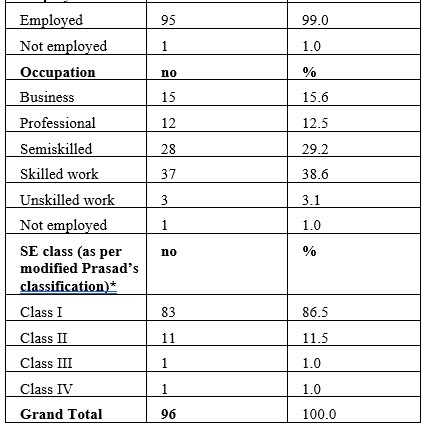
* AICPI (For Month of Sep- 21) =123.3, MF = AICPI * 4.93*4.63*2.88 /100 (Base Year - 2016) =81.06
- Because of the higher SE class, young people may have more tendency to eat junk food/packaged food. Along with a sedentary lifestyle, they pose a greater risk for CHD.
- Chest pain was the most common feature seen in about 76% of subjects in this study. Contrary to our finding, a review article* on MI ni young, showed that 69% of patients less than 45 years of age with MI, denied any chest pain before MI.
- No other study was found to have details on presenting complaints. In our study, the majority of the patients presented with a symptom complex of chest pain with oedema of feet/ breathlessness/ perspiration /vomiting/ left arm or shoulder pain. (table 3)
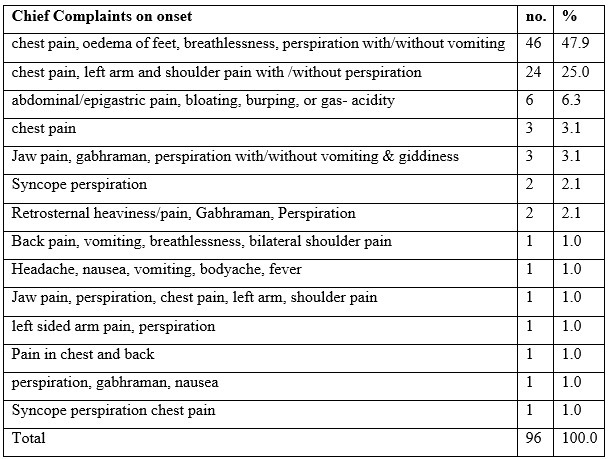
Table 3 Clinical features at the onset of MI (n=96)
- Overall, more than 80% of the patients had single coronary vessel involvement in our study. Nearly half of the patients had left coronary artery involvement either LAD or LCA followed by right coronary artery involvement (RCA) (table 4).
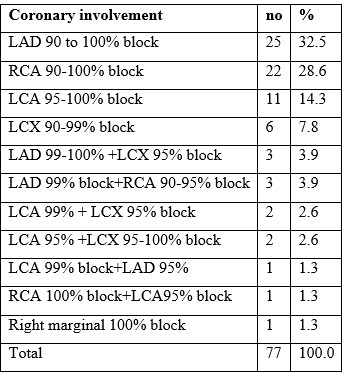
Table 4 Coronary involvement among those who undergone angiography (n=77)
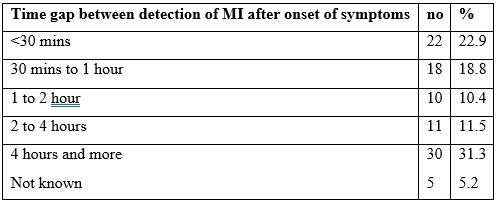
Table 5 Time gap between detection of MI after onset of symptoms (n=96)
- These findings were similar to other studies [4],[15],[1]. In this study, every patient had more than 90% coronary artery blockage in their AMI indicating all of them had Transmural myocardial infarction indicating ST elevation MI (STEMI).
- In the management of MI, the first hour is considered the golden hour. About 40% could be diagnosed in one hour in our study. The prognosis is good when reperfusion is done as soon as possible.
- According to study 3, individuals who present within two hours of the onset of symptoms are much more likely to benefit from fibrinolytic therapy than those who present later.
- The mean time gap from the onset of symptoms to diagnosis of MI in our study was around 2 hours with SD of around 2 hours (129.28 minutes 131.86 minutes). However, almost one-third of patients could be diagnosed after 4 hours or more. The mean time of presentation after symptom onset was quite long which is 16.9 hours in the AMIYA study. [4]
- The majority of the patients did not have any history of previous MI/heart problems which is 87.5% which indicates young patients directly develop MI. while in older age groups, previous angina, MI or vascular problems are frequent? [4]
- Of the minority patients who had any history of previous MI/heart problems (12.5%), 58.3% patients had angina attacks (2-5 years ago). (Table 6.1)
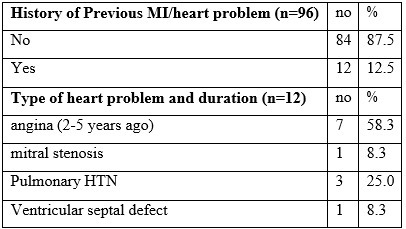
Table 6.1 History of Previous MI/heart problem
- The majority of the patients had a history of smoking.Smoking was a major risk factor in many other studies also°, [10],[12],[14],[17],[18], Around 15/*TM patients had a history of alcohol consumption.
- 42.7% of the patients used to consume chewable tobacco (Table 6.2). Tobacco is a known risk factor for cardiovascular diseases.
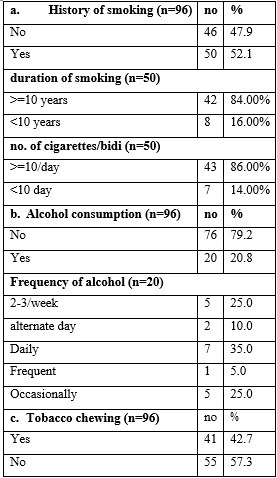
Table 6.2 Various habits among study subjects
- Nearly half had an abnormal lipid profile. (table 6.3) Abnormal lipid profile can lead to the deposition of cholesterol and lipid in the major blood vessels of the body increasing the risk of thrombo-embolic events predisposing to AMI.
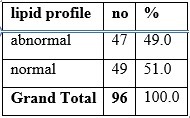
Table 6.3 Lipid profile
- 52.1% of the patients were obese or overweight (as per BMI) no patient was underweight and more than 50% of the patients frequently consumed outside food and packaged food (table 6.4 & 6.7). These food products have increased calorie content and contain Trans fatty acids which lead to an increase in LDL and can lead to overweight.
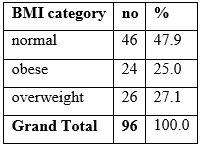
Table 6.4 nutritional status
- Overweight and obese patients are predisposed to having lipid abnormalities and also have an increased risk of comorbidities like HTN and diabetes leading to blood vessel wall damage and insulin resistance leading to metabolic disorders.
- Higher BMI and abnormal lipid profiles in young MI patients were also seen in other studies. [10],[11],[16],[18]
- 2/3rd of patients had a stressful psychological condition which is 66.7%. (table 6.5) Stress leads to an increase in the release of catecholamines including epinephrine and norepinephrine leading to an indirect increase in blood pressure which predisposes to MI.
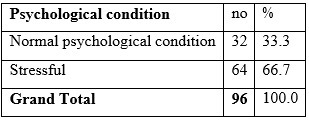
Table 6.5 Psychological condition of study subject at the time of MI episode
- A positive family history of MI was present in nearly 3/4" of the patients, or 74% (table 6.6). This was the most common risk factor found in our study (figure 3). This indicated a strong hereditary relation of AMI in young. Positive family history as a major risk factor was also mentioned by other studies. [10],[11],[13],[18]
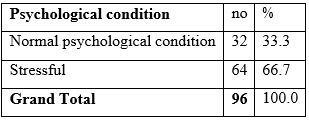
Table 6.6 Presence of family history of MI
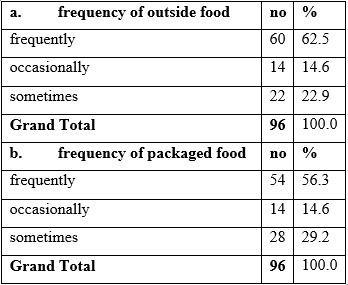
Table 6.7 Dietary habits for outside and packaged food among study subjects
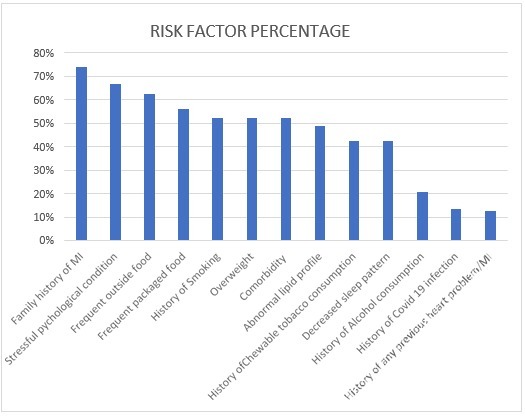
Figure 3 Percentages of various risk factors found in the study
- More than half of the patients had some type of comorbidity, out of which the majority of the comorbid patients had DM or HTN or both that is 80% of the comorbid patients. (table 6.8) These both are proven risk factors for cardiovascular diseases. Other studies have also mentioned DM &HT as common risk factors among the young.? [1],[6]
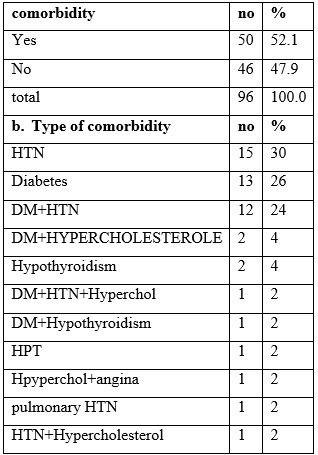
Table 6.8 Presence of comorbidity among study subjects
- Only a few (13.5%) patients had a history of COVID-19 infection, out of which 84.6% of patients developed AMI after COVID-19 infection and the rest developed AMI during COVID-19 infection.
- Patients who developed AMI after COVID, most of them developed it within a month of COVID-19. (table 6.10). Many studies [20],[21] show that there is an increase in thromboembolic events post-COVID-19 which can lead to an increased risk of AMI.
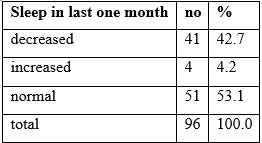
Table 6.9 Sleep pattern in the last month preceding the episode of MI
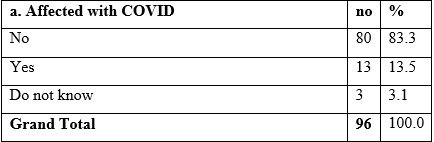
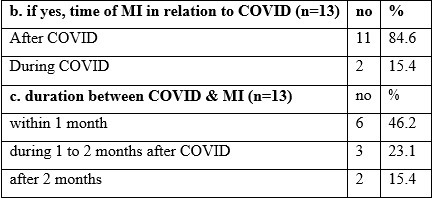
Table 6.10 History of COVID-19 and time gap with episodes of MI
Result and conclusion
This cross-sectional study on AMI of young people found that males are commonly affected. It is more common in the age group of above 35 years. Most of them were from higher socio-economic class and involved in skilled/professional work.
In the majority, it affected single coronary vessels mainly the left coronary. The most common symptom is chest pain. Less than half of patients could be diagnosed within one hour.
Common risk factors seen in descending order were a family history of MI followed by:
- Stressful psychological conditions
- Frequent outside and packaged food
- Smoking
- Overweight and the presence of comorbidity
Further analytical study is required to confirm these findings and to study the prognosis.
Limitations of the study
As there was no control group in the study, the association of risk factors could not be found.
Summary
Background and Objectives
As per RGI, Cardiovascular diseases are the top Causes of Death in the age group of 30-69 years in India accounting for about 32% of total deaths in 2010-13.
Presentation and risk factors of MI may vary in young as compared to old. In that view, the present study was conducted to study the clinical manifestations, coronary artery involvement and risk
factors of acute myocardial infarction in patients between the age of 18-50 years.
Methodology:- The study covered 96 patients who were interviewed personally as per the predesigned questionnaire to collect various demographic data and possible risk factors associated with MI. The data obtained was analysed by MS Excel 2013.
Results
The majority of the patients were male(88.5%) and were in the age group 36-50 years(84.4%). Chest pain was the most common feature in about 76% of subjects.
The majority of the patients had single coronary vessel involvement (84.5%), of which LAD/LCA blockage was the most common. All patients had>90% coronary artery blockage.
The majority of the patients had a time gap of 4 hours or more from the onset of symptoms to the detection of MI. Various risk factors found in the study were:
- Family history of MI (74%).
- Stressful psychological conditions (66.7%).
- Frequent outside food (62.5%).
- Packaged food (56.3%).
- History of smoking, overweight and comorbidity (each 52.1%) in descending order.
- The commonest comorbidity was hypertension &/or diabetes (80%).
- 13.5% of patients suffered from COVID-19 infection, out of which 84.6% of patients developed AMI after COVID-19 infection. Patients who developed AMI after COVID, most of them developed it within a month of COVID-19.
Conclusion
Chest pain was the most common symptom. Single vessel involvement especially Left coronary involvement was the commonest. Risk factors in descending order were a family history of MI followed by stressful psychological conditions, frequent outside and packaged food, smoking, being overweight & presence of comorbidity.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Kaumil Modi has an MBBS from GMERS Medical College and Civil Hospital, Ahmedabad.
Co-Author: Dr. Krimaben Indravadanbhai Patel has an MBBS from GMERS Medical College and Civil Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries