Acute Kidney Injury: Evaluation & Management
M3 India Newsdesk May 25, 2023
Acute Kidney Injury (AKI) is a condition where the kidneys suddenly stop functioning normally. It can cause anything from a slight decline in kidney function to total renal failure. This article explains the diagnosis, evaluation and management of AKI.
Acute Kidney Injury (AKI) refers to an abrupt decrease in kidney function resulting in the retention of urea and other nitrogenous waste products and in the dysregulation of extracellular volume and electrolytes. The term AKI has replaced Acute renal failure (ARF).
Definition
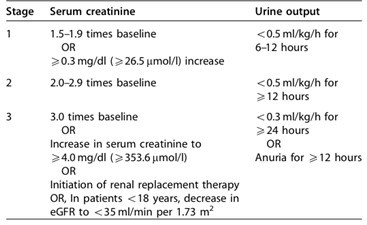
The KDIGO guidelines define AKI as follows:
- Increase in serum creatinine by > 0.3 mg/dL within 48 hours, or
- Increase in serum creatinine to > 1.5 times baseline, which is known or presumed to have occurred within the prior seven days, or
- Urine volume <0.5ml/kg/hour for six hours
This is the AKI definition by 2012 KDIGO guidelines and an update is set to be released before the end of 2023.
The KDIGO criteria allow for the correction of volume status and obstructive causes of AKI prior to classification. Serum creatinine and urine output are markers of excretory function only and do not provide any information about any other roles of the kidney, i.e. metabolic, endocrine, or immunological functions.
Staging of AKI
Evaluation
The clinical evaluation of AKI includes the following:
History taking- Careful detailed history taking is the utmost important thing in diagnosing AKI. Especially Drug history including over-the-counter formulations, NSAIDS and herbal remedies or recreational drugs. History of Lower urinary tract symptoms and nocturia should always be asked. History of heavy exercise for rhabdomyolysis. Past history of UTI and renal calculi.
Physical examination-
- It should include an evaluation of fluid status whether the patient is hypovolemic, euvolemic or hypervolemic.
- Skin turgor, dryness of the tongue and examination for pedal and sacral oedema should be a part of the examination.
- Peripheral pulses should always be checked.
- Any signs of rashes especially in cases of vasculitis or other auto-immune conditions.
- Signs for acute and chronic heart failure, and infection.
Laboratory tests-
- Renal function studies: Increased ratio of BUN to creatinine > 20:1 suggests prerenal AKI.
- Complete blood count: Elevated WBC can indicate infection; risk-stratify for tumour lysis syndrome in an oncologic patient; low haemoglobin can suggest acute blood loss or chronic anaemia; thrombocytopenia might indicate thrombotic microangiopathy or portal hypertension.
- Peripheral smear: Schistocytes may indicate HUS or TTP.
- Serologic tests: May show evidence of systemic diseases associated with AKI, such as lupus nephritis, ANCA vasculitis, anti-GBM disease or Goodpasture syndrome.
- Complement testing: Pattern may indicate AKI related to endocarditis or various glomerulonephritidites.
- Fractional excretion of sodium and urea to differentiate between Pre-renal and Renal AKI.
- Biomarkers: neutrophil gelatinase-associated lipocalin, kidney injury molecule-1, and IL-18.
USG KUB- It helps in providing information regarding obstructive uropathy and also about the size of the kidney with its cortical echogenicity and cortical thickness.
Kidney biopsy- This can be useful in identifying intrarenal causes of AKI and directing targeted therapy. It is especially helpful in rapidly progressive glomerulonephritis to determine the underlying aetiology.
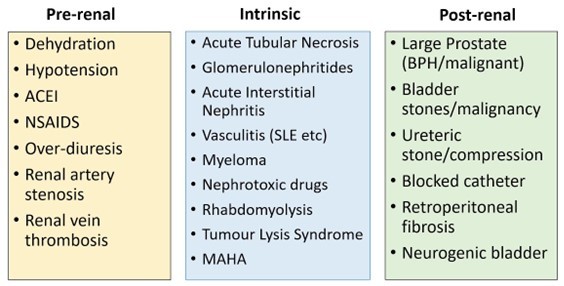
AKI can be broadly divided as follows: (including etiologies)
Management
Measures to correct underlying causes of acute kidney injury (AKI) should begin at the earliest. Serum creatinine does not rise until a large proportion of the renal mass is damaged; because the relationship between the glomerular filtration rates (GFR) and the serum creatinine level is not linear, especially early in the disease. Indeed, the rise of serum creatinine may not be evident before 50% of the GFR is lost.
The current treatment for AKI is mainly supportive in nature; no therapeutic modalities to date have shown efficacy in treating the condition.
Prevention
- Maintaining volume status and mean arterial pressure to maintain renal hemodynamics.
- 0.9% normal saline is preferred for volume resuscitation.
- Albumin is safe, albeit no more effective than isotonic saline for fluid resuscitation. However, it may be preferred in hypo-albuminemia with good urine output.
- Lonotrope support as required should be given to maintain adequate MAP for good renal perfusion.
- Appropriate use of vasoactive agents can improve kidney perfusion in volume-resuscitated patients with vasomotor shock. The preferred ionotropic is nor-adrenaline followed by vasopressin if needed.
- In patients having cardiac dysfunction with no acute myocardial event, dobutamine will help to prevent the cardio-renal syndrome.
- Avoid using nephrotoxic agents like aminoglycosides and NSAIDS.
- Avoid procedures which require intravenous contrast.
- If contrast is required to be given; prefer using low molecular weight contrast and stop diuretics and metformin prior to it.
- Also in the setting of established AKI stop ACE-/ARB and SGLT-2 inhibitors.
Treatment
- There is no specific treatment for AKI; it actually is based on identifying the aetiology and treating the specific cause which has led to AKI.
- In Pre-renal AKI, largely maintenance of hydration and maintaining MAP is the standard of care.
- The use of isotonic saline as the standard of care for intravascular volume expansion to prevent or treat AKI is based upon the lack of clear evidence that colloids are superior.
- It is acknowledged that colloids may be chosen in some patients to aid in reaching resuscitation goals, or to avoid excessive fluid administration in patients requiring extensive volume resuscitation, or in specific patient subsets (for example, a cirrhotic patient with spontaneous peritonitis, or in burns).
- The choice of crystalloid with altered tonicity is generally dictated by goals other than intravascular volume expansion (for example, hypernatremia or hyponatremia). The isotonic saline solution contains 154 mmol/l chloride and when administered in large volumes will result in hyperchloremia.
- In the absence of hemorrhagic shock, using isotonic crystalloids rather than colloids (albumin or starches) as initial management for expansion of intravascular volume in patients at risk for AKI or with AKI.
- Protocol-based management of hemodynamic and oxygenation parameters to prevent the development or worsening of AKI in high-risk patients in patients with septic shock.
- Maintaining nutrition and glycemic control is also important: Observations in critically ill patients provide a rationale to maintain a total energy intake of at least 20 kcal/kg/day but not more than 25 to 30 kcal/kg/day.
- Diuretics should be avoided except in cases of volume overload. Dopamine, fenoldopam and ANP have no proven significance.
Indications for Hemodialysis:
- Uremic encephalopathy or pericarditis
- Refractory hyperkalemia
- Refractory Acidosis
- Hypervolemia with pulmonary oedema
- Certain drug overdose
Choice of the modality of hemodialysis:
- In the setting of AKI with hemodynamic instability, CRRT is preferred rather than conventional hemodialysis. SLED i.e. Sustained low-efficiency hemodialysis can also be done if CRRT is unavailable.
- Early vs. Late initiation of dialysis: There is a lot of difference in data regarding this and it should be individualised according to the patient.
In the setting of Intrinsic Renal causes like vasculitis and other auto-immune; steroids, immunosuppressants and plasma exchange will help in the rapid recovery of AKI. In post Renal AKI, relieving obstruction by placing a Foleys catheter or D.J. stenting in obstructive renal disease of a single kidney potentially recovers AKI rapidly.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Bhavin Mandowara is a practising nephrologist at Zydus Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries