Alternative to Aspirin: Novel Insights from a New Study
M3 India Newsdesk Oct 26, 2023
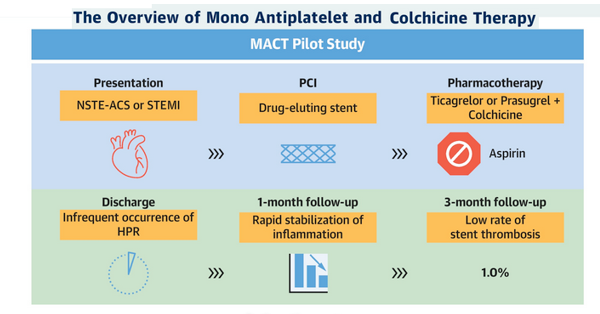
The article explores a pilot study suggesting that switching from aspirin to colchicine after PCI in ACS patients might decrease the risk of blood clots without raising the risk of bleeding.
The gold standard of treatment to avoid thrombotic events in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI) has been dual antiplatelet therapy (DAPT), which consists of aspirin plus a P2Y12 inhibitor.
According to a recent pilot trial published in JACC: Cardiovascular Interventions, aspirin may be stopped the day after PCI, and colchicine, an anti-inflammatory drug, can be administered to minimise the risk of ischemic events in these patients while lowering the aspirin's higher risk of bleeding risk.
The day after PCI, low-dose colchicine was given to ACS patients with drug-eluting stents (DES) together with maintenance treatment with a P2Y12 inhibitor (ticagrelor or prasugrel). The usage of aspirin was stopped. Only 1 patient had excessive platelet reactivity at 3 months, and only 1% of the patients had stent thrombosis.
Additionally, after 1 month, both platelet reactivity and high-sensitivity C-reactive protein (hs-CRP) decreased, suggesting that inflammation had subsided. This strategy is linked to favourable platelet function and inflammatory profiles.
Safeguarding effectiveness without compromise
The first anti-inflammatory medication proven to lower the risk for myocardial infarction, stroke, coronary revascularisation, and cardiovascular death in adult patients with either established atherosclerotic disease or multiple risk factors for cardiovascular disease is colchicine 0.5-mg tablets, which we Food and Drug Administration recently approved. It aims to combat persistent inflammation, which is thought to be the root of cardiovascular events.
Patients undergoing PCI are often treated with DAPT. Still, given the risk for increased bleeding associated with aspirin, particularly when taken long-term there is a "need to identify strategies associated with a more favourable safety profile without compromising efficacy," the authors write.
The termination of aspirin medication after one to three months and the maintenance of P2Y12 inhibitor monotherapy have both been studied in the past, with varying degrees of success. Colchicine, however, was shown in one study to be helpful in decreasing recurrent ischaemia, and its advantages may be enhanced with early induction in the hospital.
"Strategy that substitutes aspirin with colchicine during the acute phase to maximise the treatment effect of reducing recurrent ischaemia and bleeding."
- According to the new study authors
To test this strategy, the Mono Antiplatelet and Colchicine Therapy (MACT) single-arm, open-label proof-of-concept trial was created.
The study involved 200 patients who underwent PCI with DES with non-ST-segment elevation ACS and ST-segment elevation myocardial infarction (STEMI) and received either ticagrelor or prasugrel along with a loading dose of aspirin (mean [SD] age, 61.4 [10.7] years; 90% male; 100% Asian ethnicity).
Aspirin was stopped the day after PCI, and low-dose colchicine (0.6 mg once a day) was also given along with the P2Y12 inhibitor. Staged PCI was carried out while colchicine and ticagrelor or prasugrel were being maintained.
No further antiplatelet or anticoagulant medications were allowed.
Before being released, patients had their platelet function checked using the VerifyNow P2Y12 assay. At admission, 24 and 48 hours after PCI, as well as at the 1-month follow-up, hs-CRP levels were assessed.
A clinical follow-up was done after one and three months.
- Stent thrombosis within three months of follow-up was the primary outcome.
- Secondary outcomes were changes in hs-CRP levels between 24 hours after PCI and 1-month follow-up, all-cause mortality, MI, revascularisation, significant bleeding, and a composite of cardiac death, target vessel MI, or target lesion revascularisation.
How inflammation plays a part
- The whole procedure was followed by 190 of the first 200 patients, making them eligible for follow-up. There were just two patients who experienced the main consequence. It was discovered that one of the patients had not taken her antiplatelet medication consistently.
- Although there was bleeding in 36 individuals, just 1 patient had a significant haemorrhage, according to the investigators. At discharge, the platelet reactivity level was 27 42 PRUs.
- Only 0.5% of patients matched the criterion for strong platelet reactivity, whereas the majority of patients (91%) did. Whether the patients were on ticagrelor or prasugrel, platelet reactivity was the same.
- After one month, the hs-CRP level dropped from 6.1 mg/L (interquartile range [IQR], 2.6 - 15.9 mg/L) at 24 hours after PCI to 0.6 mg/L (IQR, 0.4 - 1.2 mg/L; P .001).
- In all patients, the amount of inflammation was "reduced considerably" over time. At 24 hours after PCI, the prevalence of high inflammation criteria—defined as hs-CRP 2 mg/L—was 81.8%; at 1 month, it was 11.8% (P .001). They note that major bleeding was uncommon, with a 3-month frequency of 0.5%.
"Inflammation plays a fundamental role in the development and progression of the atherothrombotic process."
- According to the authors
The acute phase of MI is also characterised by "an intense inflammatory response" that is brought on by a number of reasons and may result in unfavourable myocardial remodelling. In the current trial, inflammation levels dropped quickly.
They identified various drawbacks. For instance, all of the included patients were Asian and had reduced ischaemia and bleeding risks. "Although ticagrelor or prasugrel is effective regardless of ethnicity, clinical data supporting this de-escalation strategy are limited," they claim. Furthermore, there was no control group to use as a benchmark. They conclude that the results need further research.
Promising but preliminary
"Too soon for extensive clinical translation of these findings."
- According to some experts
Larger and more thorough randomised studies, on the other hand, are "on their way to give more precise estimates regarding the risks and benefits of early aspirin withdrawal in ACS."
- In this situation, early colchicine addition seems to provide the best chance of reducing possible thrombotic risk without raising bleeding risk.
- The trial provides novel insights on early aspirin withdrawal and P2Y12 monotherapy in an unselected population including [those with] STEMI.
- The results could be fascinating for those patients at extremely high bleeding risk or who are actually intolerant to aspirin a situation in which options are constrained.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monish Raut is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries