“50% patients undiagnosed”: COPD Treatment guidance by Dr. Jyotsna Joshi
M3 India Newsdesk Nov 21, 2018
On World COPD Day 2018, Dr. Jyotsna Joshi, a renowned Pulmonologist discusses the pathogenesis and treatment guidance for the disease.

World Chronic Obstructive Pulmonary Disease (COPD) Day is a global effort to boost people’s understanding of COPD and advocate for better care of patients. It falls on the second or third Wednesday of November and this year.
COPD is a group of progressive lung diseases that obstruct airflow.
- With an estimated disease burden of 210 million people worldwide,
- COPD was the fourth leading cause of death (5.1%) in 2004 and is projected to occupy the third position (8.6%) in 2030.
- The prevalence of COPD in adults ranges between 0.2% in Japan and 37% in the USA.
- In India, the BOLD study conducted in Pune, Mumbai, and Srinagar reported overall COPD prevalence estimates of 6.25%, 6.8%, and 16.05%, respectively.
COPD Terminology
COPD is used in 2 different ways:
- Smoking-Related Chronic Airflow Limitation (CAL)
- All causes for CAL
- Smoking-related CAL
- Chronic asthma with fixed airway obstruction
- Bronchiectasis
- Cystic fibrosis
- Sequelae of Tuberculosis
- Obliterative bronchiolitis
- Others
COPD: Risk Factors
- Cigarette smoke the most common risk factor
- Biomass fuel exposure
- Occupational exposure
Biomass fuel exposure in women who use “Chullah” for cooking has been found to be an important cause for COPD in India.
COPD: Definition
- History of smoking >10 pack years
- Symptoms of chronic airflow limitation
- FEV1/FVC %<70% and FEV1% predicted <80%
- Poor or no bronchodilator reversibility
Note: Specific causes of chronic airflow limitation such as cystic fibrosis, bronchiectasis and obliterative bronchiolitis (OB) should be excluded.
COPD: Susceptibility to smoke
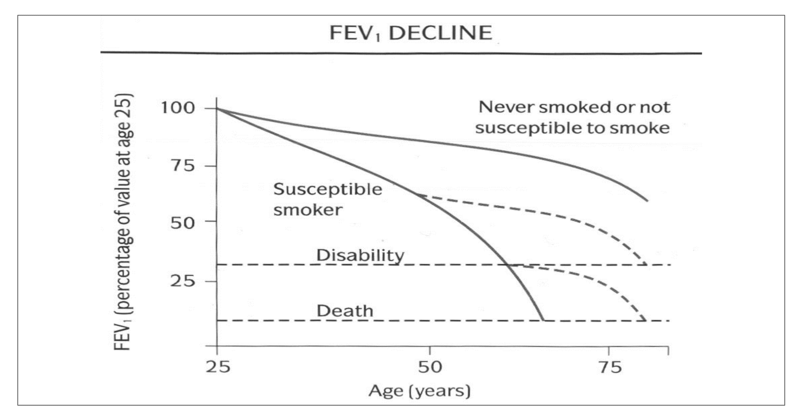
COPD Pathogenesis
- Only 50% of all chronic smokers develop the disease.
- AAT is a known genetic defect, but occurs in <1% of individuals with COPD
- Gene Polymorphisms reported in COPD are:
- Polymorphisms of p53 and p21 genes
- Genetic polymorphism of the group-specific component of serum globulin (Gc-globulin), also known as vitamin-D-binding protein
- Alpha-defensins are major constituents of neutrophil granules, and beta-defensins, expressed in airway epithelial cells
- Two different beta-defensin-1 polymorphisms have been associated with chronic obstructive pulmonary disease phenotypes In Japanese and Chinese populations
Differentiating COPD from Asthma
Similarities that exist:
- Chronic inflammatory diseases causing airflow limitation
- Complex interaction of hereditary factors and environmental stimuli.
- Gene-environment interaction (allergens for asthma vs. individual smoking for COPD)
- Genome-wide screen results linkage to chromosome 2q in both asthma and COPD
- Candidate gene association studies for IL-13 in both asthma and COPD populations
Differences between COPD and asthma
- Asthma
- Intermittent symptoms
- Family history of atopy
- Childhood onset
- Significant reversibility in FEV1
- Dramatic and excellent response to inhaled steroids
- COPD
- Slowly, progressive symptoms
- History of tobacco smoking
- Onset after 40 years
- Poor FEV1 reversibility
- Inadequate response to inhaled steroid
Asthma Treatment Scheme
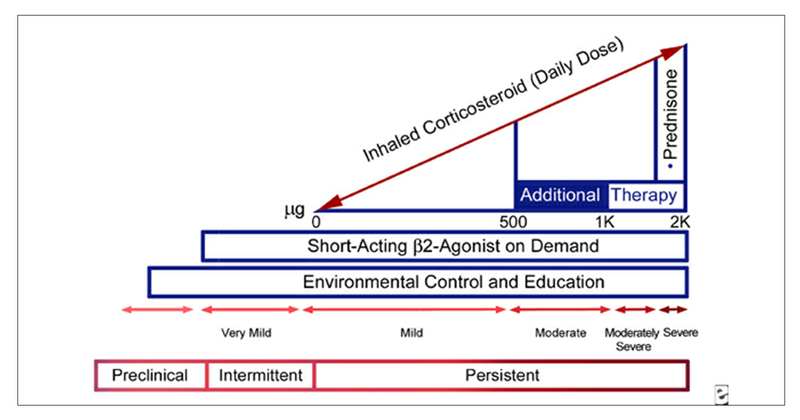 Asthma COPD overlap (ACO) is when features of both disorders overlap. Such patients are treated for asthma.
Asthma COPD overlap (ACO) is when features of both disorders overlap. Such patients are treated for asthma.
COPD mimic: Postinfectious Obliterative Bronchiolitis (OB)
OB occurs due to obstruction of the small airways. There are numerous causes for OB but in India, post infectious particularly post-tuberculosis (TB) commonly called post TB COPD is very common. The symptoms mimic that of COPD but occur in non-smoking young individuals.
Turton's clinical criteria include:
- Symptoms of CAL
- Reduced FEV1
- Exclusion of known causes of CAL
HRCT showing mosaic perfusion clinches the diagnosis.
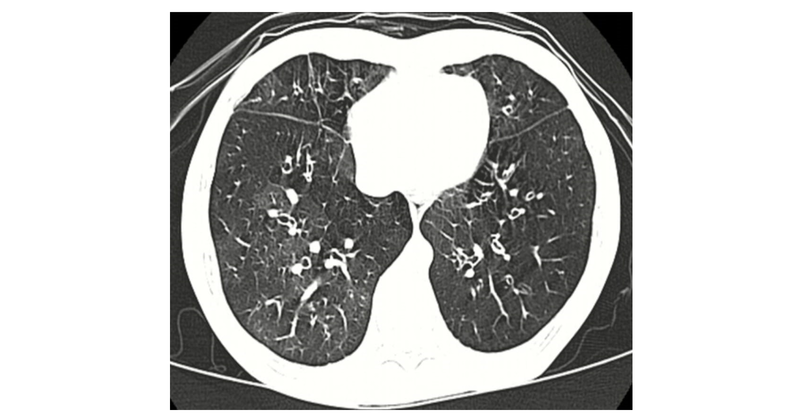
Figure showing tile like “mosaic” pattern
Treatment is same as for COPD, however, oral bronchodilators may be more beneficial as inhalers may not reach the small airways.
COPD: A systemic disease
COPD is now considered as a systemic disease due to multiple associated comorbidities.

1. COPD has been consistently associated with an increased risk of lung cancer. However, previous studies have had limited ability to determine whether the association is due to smoking. Inflammatory processes may both contribute to COPD and be important for lung carcinogenesis.
2. Anxiety and depression are very common comorbidities in COPD and have a significant impact on patients, their families, society, and the course of the disease.
COPD: Sarcopenia
- Patients may be overweight (Blue Bloater) or underweight (Pink Puffer) Skeletal muscle loss is common in both due to oxidative stress, excessive work of breathing and poor appetite-anxiety/depression.
- It has long been known that cigarette smoking is a potent risk factor for atherosclerotic disease as well as for COPD. Overall, 40% of COPD patients have at least one of these vascular (cardiovascular, cerebrovascular) comorbidities.
- COPD patients have an increased risk of and peripheral artery disease related to tobacco smoking and severity of COPD. May affect the 6-min walk test performed to assess physical exercise capacity. Peripheral arterial dysfunction must be considered in the multidisciplinary treatment of these patients.
- The metabolic syndrome is a cluster of risk factors (abdominal obesity, hypertension, dyslipidaemia, and insulin resistance). In one study, almost ½ of the patients with COPD had coexisting metabolic syndrome. Was associated with an increase in the levels of some systemic inflammatory markers (high-sensitivity C-reactive protein [hs-CRP], interleukin-6, fibrinogen) and physical inactivity, independent of PFT.
- OSA and COPD are both prevalent (2%-4% and 15% respectively). Overlap occurs in 1% adults. OSA and COPD share risk factors: male gender, age, cigarette smoking, and systemic inflammation. Control of breathing defect may predispose to OSA.
- Studies show that GERD is more common in patients with COPD than in those without the condition. COPD exacerbations may be associated with GERD. Improvements in respiratory symptoms observed in patients receiving acid-suppressive therapy for GERD.
Treatment of COPD
Comprehensive Management of COPD
- Smoking cessation/avoidance of offending agent
- Pharmacotherapy
- Rehabilitation including long-term oxygen therapy (LTOT)
- Treatment of Anxiety/ Depression, Osteoporosis, Sarcopenia, AD, Metabolic syndrome GERD and OSA.
- Surgery
Smoking Cessation
- Simple advice: Each year about 1% quit from own initiative and simple brief advice from a clinician increases this up to 3%
- Written self-help materials
- Individual and group behavioural support which can increase cessation to about 7%
Smoking Cessation: Pharmacotherapy
Nicotine replacement therapy (NRT): Nicotine gums, patches, and sprays when used with an intensive behavioural program, nicotine replacement may increase rates of quitting up to two-fold. Without a behavioural program, quit rates with gum are lower. Treatment is generally recommended for 3 to 6 months.
Drugs for smoking cessation
- Bupropion
- Dose- 150 mg usually daily for 7 days, then twice daily for 7 -12 weeks
- Precautions: Rarely causes seizures, but should not be used in patients with seizure disorder, head trauma, heavy alcohol use, anorexia nervosa, or bulimia
- Varenicline
- Dose- 0.5 mg once for 3 days, then 0.5 mg twice for 4 days, followed by 1 mg a day for 12 weeks
- Side effects- Depression, suicidal behaviour
Pharmacotherapy in COPD
Pharmacotherapy is prescribed based on the severity of COPD. This is called combined assessment scoring based on symptoms and exacerbations.
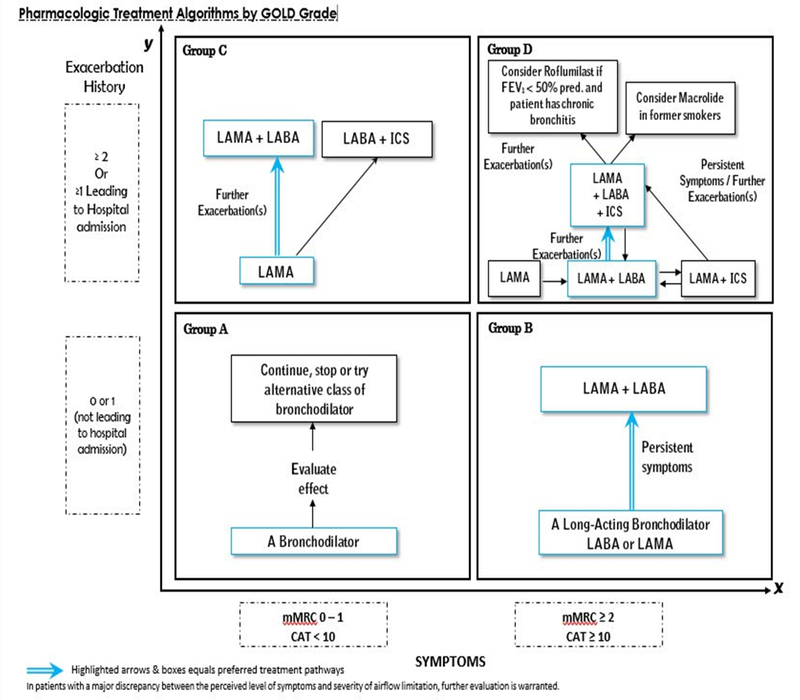
- LABA+ ICS, but not LAMA are individually associated with a reduction in the decline of lung function. The only therapy associated with a reduction in mortality as well as a reduction in the decline in lung function was LABA+ ICS.
- Triple therapy has additional benefits. Therefore, in a patient with early disease- only SABA, LABA, LABA+ LAMA or ICS+LABA is recommended. In patients who have uncontrolled COPD or patients who have severe disease, ICS+LABA+LAMA is recommended.
- Phosphodiesterase inhibitor PDE4, Roflumilast is recommended for patients who have frequent exacerbations. In India, low dose sustained-release theophylline or deriphyllin works equally well. In low doses, the safety concerns are not relevant.
Long-term oxygen therapy (LTOT) in COPD
Low flow oxygen for 15-17 hours per day improves quality of life (QOL), neuropsychiatric symptoms, improves pulmonary hypertension and Cor pulmonale (right heart dysfunction) and mortality.
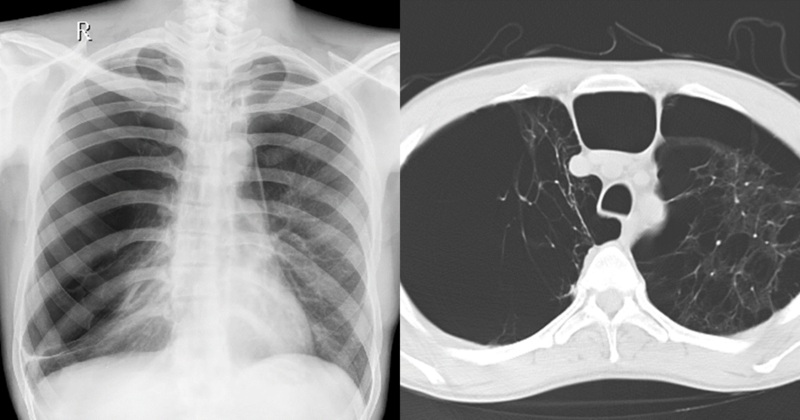 CXR and HRCT showing giant bulla and diffuse emphysema
CXR and HRCT showing giant bulla and diffuse emphysema
Surgery in COPD
- Bullectomy
- Lung volume reduction surgery
- Lung transplant
COPD: Predicting the risk of mortality- The BODE Index
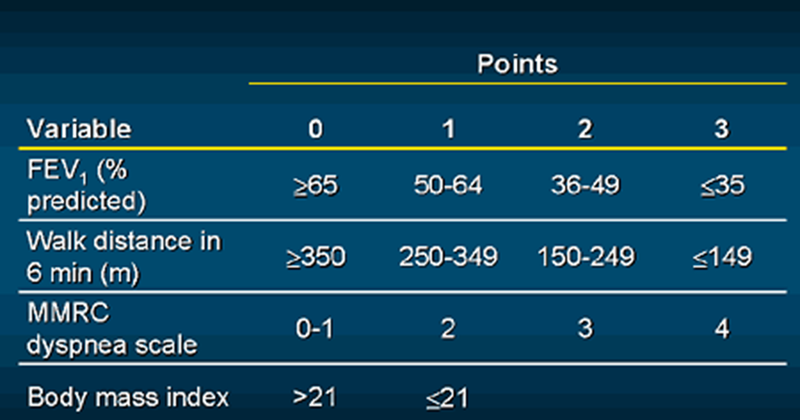
The BODE index, BMI (body mass index), Obstruction (FEV1), Dyspnoea and Exercise tolerance is better than the FEV1 at predicting the risk of death from any cause and from respiratory causes among patients with COPD.
COPD Rule of 50s
- 50% COPD patients remain undiagnosed
- COPD is evident by age 50
- At the time of diagnosis FEV1 is usually 50%
- Diseases has a 50% 5-year survival rate
However, as this year's world COPD day slogan says it is “never too early, never too late” to diagnose and treat COPD.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries