General practice series - Common skin lesions in children: Dr. Balaji Chinnasami & Dr. Janani Arul
M3 India Newsdesk Apr 28, 2020
Dr. Balaji Chinnasami and Dr. Janani Arul, in this series, provide assistance to general practitioners in treating infants and children with skin infections by providing ready-made evidence-based prescriptions.

ATTENTION: Images in this article contain pictures of patient presentation which some people may find offensive or disturbing. Viewer discretion is advised.
Seborrheic dermatitis
An 8-week old baby presents with raised, scaly, greasy patches on his scalp.

Science behind management
Seborrheic dermatitis is a benign self-limited condition common in infants and adolescents. It is a clinical diagnosis. It is characterised by greasy, yellow, scaly sometimes erythematous lesions with mild pruritis present on regions with a large number of sebaceous glands like the scalp (cradle cap), face, post auricular area, genitals, chest, and back.
- Skin changes could be the result of inflammatory response to Malassezia yeast.
- Emollients and shampoos should be the initial treatment followed by topical anti-fungal agents.
- Topical steroids are the second line treatment and should be used sparingly.
Investigations to run
It is a clinical diagnosis. In unresponsive cases alone evaluate for immunodeficiency.
Rx
Step 1: Applying emollients like petroleum jelly, mineral oil, olive oil followed by brushing and shampooing may be sufficient for mild cases. Frequent shampooing may reduce the flaking.
Step 2: For infants not responding to initial treatment
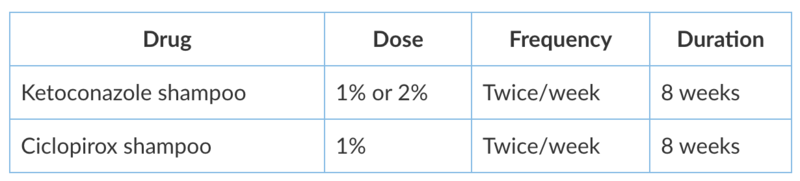
Infants not responding to the above treatment need a dermatologist referral. In older children in addition to the above steps, the below medications can be added.
Step 3: Keratolytics & Anti-inflammatory
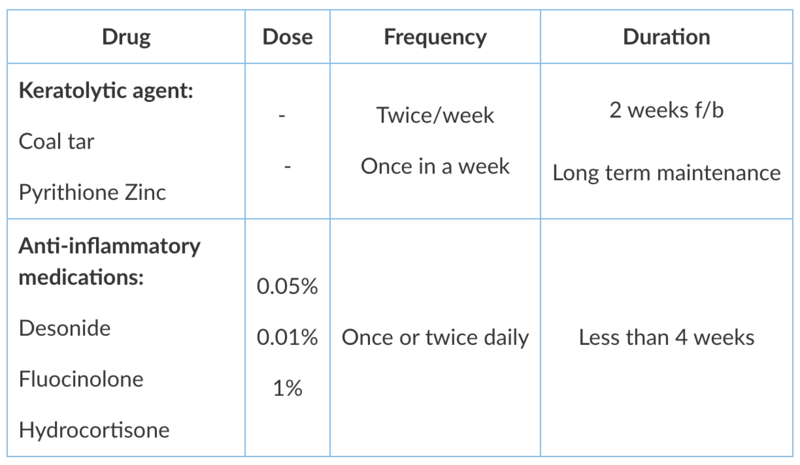
Long term maintenance treatment with antiifungal and keratolytic agent applied once a week is necessary to prevent relapse.
Advice to give to parents
- Reassure that this is a benign condition.
- Advise to apply emollients and use shampoo regularly, followed by brushing of the scalp.
Diaper dermatitis
A 6-month-old child presents with red rash in the diaper region. The child is crying a lot while changing diapers or while wiping. The child's parents often avoid changing diapers to avoid waking the child up. The child's diapers are often full when changing.

Science behind management
Diaper dermatitis is caused by increased wetness of skin due to prolonged contact with urine and faeces. This increases the penetration of irritant substances like ammonia, bile salts, harsh soaps etc resulting in irritant contact dermatitis. Cloth diapers, less frequent changes, and diarrhoea are risk factors.
- Diaper dermatitis presents as erythematous patches on convex surfaces sparing inguinal creases. Skin in the folds is spared as they don’t come in direct contact with the diaper.
- Secondary candidal infection can occur. Candida can involve inguinal creases with discrete satellite lesions and scaling along margins.
- Initial steps like application of barrier creams like Zinc oxide and keeping the diaper area clean and dry may be enough to heal.
Investigations to run
Routinely no investigations are needed. KOH mount is needed if candidal infection is suspected.
Rx
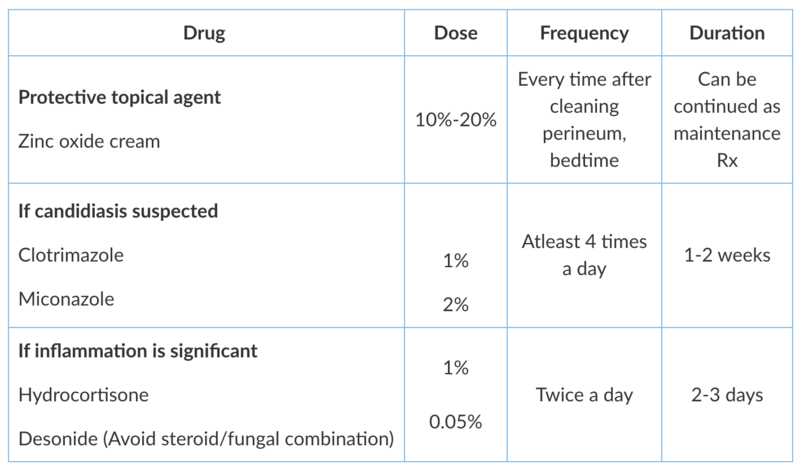
Advice to give to parents
- Change the diaper more frequently and keep the skin clean and dry.
- Use water-soaked clothes, unscented wipes, mild soaps and do gentle cleansing instead of rubbing.
- Use superabsorbent diapers instead of cloth diapers.
- Apply a bland protective topical agent like petrolatum ointment, zinc oxide or coconut oil frequently.
Urticaria
A 4-year-old child presents with itchy skin lesions for three days.

Description of skin lesions
- Intensely pruritic wheals, pale to erythematous in colour, round, polymorphic and some rapidly coalesce into serpiginous lesions.
- Lesions resolve in 24 hours and new crops reappear.
- Commonly involves face, lips, genitalia and upper airway.
Science behind management
Urticarial lesions are self-limiting and benign. It is due to release of histamine from mast cells/basophils by IgE and non-IgE mechanisms. It can be associated with oedema of subcutaneous tissues like lips, vocal cords etc. and is called angioedema.
- Urticaria can be a part of anaphylaxis. Hence, look for abnormal vital signs, cardiovascular and pulmonary symptoms. Infections, medications, insect bites, food allergens can be triggers.
- Second generation H1 antihistamines are safe and effective for control of symptoms. Twice to four times the normal dose can be given if needed.
- Steroids can be prescribed for severe cases of urticaria.
Investigations to run
Not needed but if parents insist, limited non-specific laboratory workup can be done like CBC, ESR, CRP.
Rx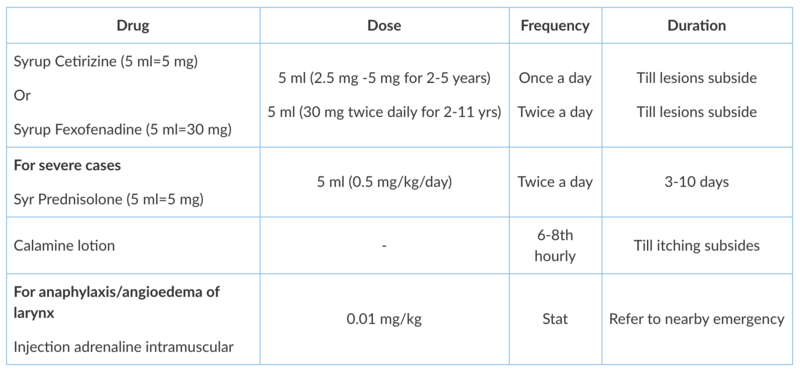
Referral
Dermatologist referral will be needed if wheals persists more than 24 hours with burning sensation and arthralgia suggesting urticarial vasculitis or if the child has chronic urticaria where lesions keep recurring for >6 weeks.
Advice to give to parents
- Avoid triggers if identified. It is the best treatment.
- Reassure that lesions will disappear and reappear and may take time to fully resolve.
- Avoid NSAIDS.
- Avoid tight clothes.
An infant with atopic dermatitis
A 10-month-old infant presents with itchy erythematous scaly lesions over the cheeks, forehead, and trunk for 3 weeks. The child is active but irritable and gets disturbed during sleep. The irritability is not associated with fever or poor feeding.

Science behind management
Atopic dermatitis (AD) is characterised by pruritis, xerosis, eczematous skin lesions and later on, lichenification.
- In infants, it presents as xerosis over the face and body and during flare ups, as erythema and exudation of regions like antecubital fossa and popliteal fossa. But sparing of the diaper area occurs.
- In toddlers, it presents as eczema and becomes localised to extensor surfaces like elbows, and knees.
- In older children, it presents as dry, scaly, itchy lesions over the elbow and knee flexors. Lichenification is characteristic of childhood AD.
- It is a clinical diagnosis and onset is usually before two years of age with a relapsing course. It has association with allergic disorders like asthma.
- Regular, liberal use of emollients is the most effective mode of treatment. Emollients with high oil content and low water content are recommended.
- Topical steroids are used for flare ups but prolonged use can result in skin atrophy.
Investigations to run
No lab tests are needed for diagnosing atopic dermatitis
Treatment
Indications for dermatologist opinion
- Patient having AD on the face and eyelids that has not responded to treatment
- Infants requiring systemic therapy for flare ups or maintenance
- Association with significant psychosocial disturbances (sleep disruption or school absenteeism)
Advice to give to parents
- Use soft fabric clothes like those made of cotton and wash them in a mild detergent. Avoid woollen garments.
- Avoid specific foods only if there is concomitant food allergy.
- Communicate with patients that treatment doesn’t cure but provides good control of symptoms.
Impetigo
A 2-year-old, 12 kg male child presents with vesiculopapular lesions with few vesicles breaking into honey-coloured crusts on the face for five days. Symptoms are not associated with itching/discharge. On examination, a few cervical lymph nodes up to 1 cm were palpable.

Science behind management
There are two types of impetigo: non-bullous (70% of cases) and bullous (30% of cases). Honey crusts on the face and extremities are the most common presentation. It is a clinical diagnosis and highly contagious.
- Topical and systemic antibiotics covering for both staphylococcus and streptococcus are the treatment of choice.
- Oral clindamycin is recommended when suspecting MRSA infection.
Lesion characteristics
- Non-bullous impetigo is characterised by honey-colored crusts on the face and extremities.
- Bullous impetigo is characterised by large, flaccid bullae mostly affecting intertriginous areas. The bullae rupture and ooze but resolve in 2 to 3weeks without scaring.
Treatment
In addition to topical antibiotics, oral antibiotic therapy is recommended when-
- Large or recurrent bullae occur
- Systemic symptoms appear
Advice to give to parents
- Maintain personal hygiene (wash child's hands and legs with soap and disinfectants), as it is effective for prevention.
- Gentlly cleanse with antibacterial soap.
- Wet dressings can also be done and are useful.
Tinea infections
A 7-year-old child is brought with itchy circular skin lesion in his leg for the past one week.

Science behind management
Tinea infections are caused by dermatophytes and are classified by the involved site. The most common infections in prepubertal children are tinea corporis and tinea capitis. Tinea versicolor (Pityriasis versicolor) is not caused by dermatophytes but rather by yeasts of Malassezia.
- Topical fungicidal agents are usually sufficient for Tinea corporis.
- Tinea capitis should not be treated solely with topical agents. Combine oral therapy with sporicidal shampoos, such as selenium sulfide or ketoconazole.
Clinical features
Investigations to run
It is a clinical diagnosis, so it does not need laboratory confirmation. In cases of atypical presentation, a KOH (Potassium hydroxide) preparation visualises the dermatophytes and aids in the diagnosis.
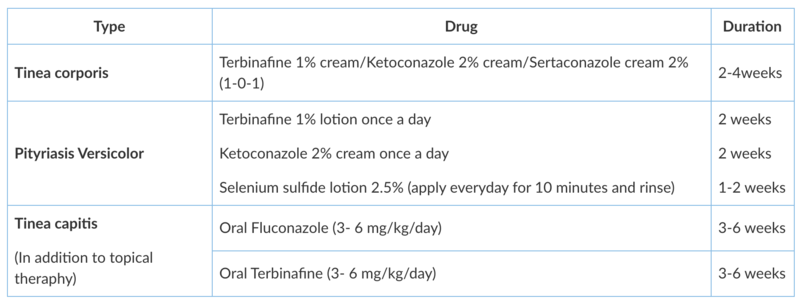
Treatment
Tinea corporis & Pityriasis versicolor- Topical therapy with azoles and allylamines is the first line of treatment.
Tinea capitis
- Requires systemic antifungals, because topical antifungals does not penetrate the hair shaft.
- Concomitant treatment with 1% or 2.5% selenium sulfide shampoo or 2% ketoconazole shampoo should be used for the first two weeks. It reduces transmission.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
Dr. Balaji Chinnasami is a Professor of Paediatrics and Medicine at a reputed medical college in Chennai.
Dr. Janani Arul is an Assistant Professor of Paediatrics from Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries