Continuous glucose monitoring for diabetes management: Dr. Jothydev Kesavadev
M3 India Newsdesk Feb 10, 2020
Dr. Jothydev Kesavadev writes on continuous glucose monitoring (CGM) system which has in recent times, become an important part of disease management in diabetes patients. In this article, he focuses on classification of CGM with merits and demerits of the system.
The global incidence; the pace of change in prevalence and mortality rates of diabetes has increased tremendously in recent times owing to our transition towards a sedentary lifestyle. Diabetes described as a group of metabolic disorders develops when the blood glucose (BG) level is out of whack over a long period. Hence, glucose monitoring plays a pivotal role in diabetes management and prevention.
The ADA-endorsed glucose meter (1987) remains the mainstream of the glucose monitoring techniques and is still considered the gold standard for home-based glucose monitoring. While glucose meter is very useful for measuring blood glucose levels, it does not enable many patients to adequately manage blood glucose levels and capture pronounced or sustained hypo/hyperglycaemic excursions.
Thus, in the mid-1970s, a novel concept termed as Continuous Glucose Monitoring (CGM) was developed as a better alternative to glucose meter which aids healthcare providers and patients to identify and manage the glucose level. [1] Gradually CGM was broadly heralded as a great advance and ADA has established Time In Range (TIR) as one of the goals in 2020.
Continuous Glucose Monitoring
CGM is a method of using a small sensor inserted into the subcutaneous tissue to measure the interstitial blood glucose (ISF) levels. In its introduction, various studies were conducted in many parts of the world, including India, to assess its potential benefits over glucose meter.
- For instance, a study of ours that analysed the effect of P-CGM on the glycaemic control of type 2 patients revealed that P-CGM gives actionable data that confirms its use in self-care practices. [2]
- Another P-CGM study of ours on FreeStyle Libre Pro (FSLP) that evaluated its clinical utility, also showed significant reductions in mean HbA1c and FBS levels in patients with diabetes. [3]
Hence, with the mounting evidence reported from the various studies on CGM, it can be considered as a better choice for glucose monitoring compared to a conventional glucose meter.
Classification of CGM
For clinical practices, two modalities are there for CGM:
- Professional/Blinded Continuous Glucose Monitoring
- Personal/Real-time Continuous Glucose Monitoring
Professional/Blinded Continuous Glucose Monitoring (P˗CGM)
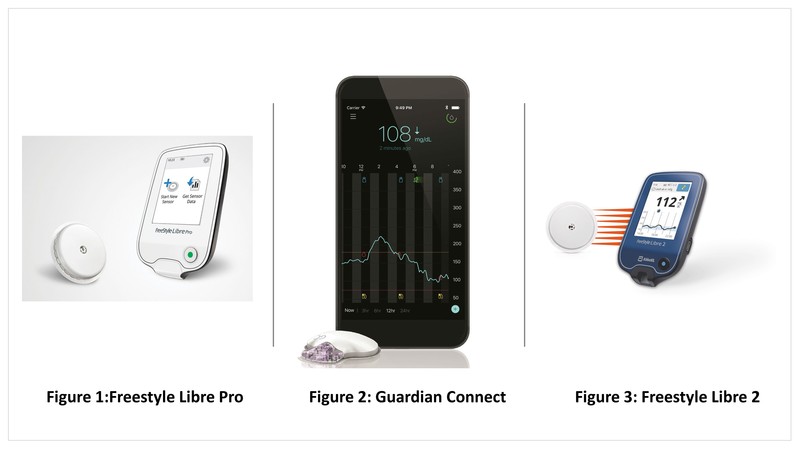
PCGM is designed exclusively for diabetes healthcare providers. It is not possible to retrieve the real-time readings from a P-CGM but can download the data from the recorded readings. The patients were supposed to wear the device for a suggested period and return to the healthcare team for further analysis of glucose profile along with backdated data. The Continuous Glucose Monitor System (CGMS) or CGMS Gold is the first P˗CGM introduced by Medtronic MiniMed which got FDA approval in June 1999. [4] FSLP is another example of a widely used P-CGM (Figure 1).
Personal/Real-time Continuous Glucose Monitoring (RTCGM)
RT˗CGM includes patient-owned devices that allow a small sensor to be placed subcutaneously to send glucose readings wirelessly, which can be viewed on a separate receiver device in real-time and continuously. This real-time data offers more knowledge about the current glucose concentration, its trend, and enables patients and healthcare providers to prevent undesirable glucose excursions. Predictive alarms are also available in some versions of the RT-CGM which alerts patients when they cross the recommended glucose targets. Examples of RT˗CGM include Eversense, Guardian Connect (Figure 2), and FreeStyle Libre 2 (Figure 3).
Intermittently scanned CGM (isCGM)
isCGM provides a continuous stream of glucose data to the user but requires an intentional sensor scan by the user to retrieve the information. The FreeStyle Libre Flash Glucose Monitoring System from Abbott Diabetes Care falls under this category. The FreeStyle Libre system employs two components: a combined glucose sensor and a separate touch-screen reader device. When the reader device is swiped nearby to the sensor, the sensor transmits a glucose level, the direction and velocity of changing glucose as well as an eight hour trend graph to the reader. If more than eight hour pass between scans, only the most recent eight hour of data will be retained and available to the user for review.
Integrated CGM (iCGM)
iCGM can integrate with other compatible medical devices such as automated insulin dosing systems, insulin pumps, blood glucose meters, or other electronic devices used for diabetes management. The ability of iCGM to operate with its compatible devices grants patients the flexibility to tailor diabetes management tools of their preferences to keep glucose levels within the permissible range. Dexcom G6, from Dexcom, the first interoperable CGM to get the designation is a typical example of an iCGM.
Components and working principle
A typical CGM consists of the following three basic parts:
- A glucose oxidase-based electrochemical sensor inserted into the patient through the skin using a needle introducer
- A transmitter that is fixed onto the sensor
- A receiver that picks up the ISF signal
The working principle of CGM is that the glucose oxidase-based sensor oxidises the interstitial fluid glucose (ISF glucose) and generates an electrical current. This electrical current carries the data regarding the ISF glucose level of a CGM user. The generated data is filtered and cleared from background noise by the transmitter. The transmitter delivers the data to the receiver which provides an approximation of the BG level, its trend, and history.
CGM Time lag
There is observed a time lag in the measurement and display of results with CGM. This time lag can be due to two factors:
- Physiological factors
- Technological factors
The physiological factors responsible for the time lag are the local blood flow, the local tissue perfusion, the permeability of ISF and the local conviction of ISF. The technological factors responsible for the time lag are the glucose diffusion through the protecting membranes and the speed of glucose reactions inside the sensor. CGM time lag can be compensated either by the calibration of the glucose sensor against the corresponding blood glucose meter readings or by the use of mathematical prediction algorithms.
CGM data reporting
The concept of Ambulatory Glucose Profile (AGP) was the brainchild of Dr. Roger Mazze from USA who first put forward the idea by interpreting glucose data in 1987. The AGP is a visual report that collates and converts all of the readings obtained from CGM into a waveform. While the waveform will start to develop after 5 days of data collection, 14 days of data collection has been considered ideal to reflect glucose control. This makes interpreting blood glucose levels much easier for both trained and untrained users.
Merits and Demerits of CGM
The merits and demerits of CGM are described in the following table.
Table1. Table shows the merits and demerits of CGM
| Merits | Demerits |
| CGM monitoring provides the data necessary for patients to make decisions related to food intake, insulin doses and physical exercise. | CGM data analysis and interpretation requires a lot of time and dedicated effort from the side of the patients and the physicians. |
| RT-CGM provides a plethora of information such as direction, magnitude, duration and causes of glucose level fluctuations that help in intensive diabetes management. | There is time lag, bio-fouling, passivation of electrodes and degeneration that could lead to a drift in the sensor signal. |
| CGM facilitates the detection of glycaemic variability associated with future risk conditions such as microvascular disease. | A minority of the users still express their inconvenience in wearing the device continuously. |
| The most notable benefit of CGM is the wealth of time-series glucose data this technology provides. | Continuous glucose monitoring devices are too expensive for patients with no healthcare funding support. |
CGM serves as an excellent tool for the appropriate management of glucose levels in patients with diabetes and will definitely replace glucose meters in the future. But for the next five to ten years, the device will remain as a better alternative to complement glucose meter. However, the use of CGM technology and CGM data interpretation requires extra effort and training for the diabetes healthcare team. But if incorporated in routine diabetes care, it will have a remarkable impact on improving its outcomes.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Jothydev Kesavadev is an acclaimed Diabetologist, and Chariman and Managing Director at Jothydev's Diabetes Research Centre, Kerala.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries