MD Anderson study shows key enzyme linked to therapy resistance in deadly lung cancer
Newswise Dec 12, 2018
Researchers at The University of Texas MD Anderson Cancer Center have identified a link between an enzyme tied to cancer formation and therapy resistance in patients with epidermal growth factor receptor (EGFR)-mutant non-small cell lung cancer (NSCLC).
They believe two existing therapies may hold promise for clinical studies for this deadly and common lung cancer for which relapse often occurs within one year following treatment. The study revealed a unique “addiction” between the enzyme protein kinase C delta (PKCδ) found in NSCLC tumors and standard-of-care treatment called EGFR tyrosine kinase inhibitors (TKIs). Based on mouse and human tissue samples, this link allows PKCδ to lessen TKIs’ ability to forestall cancer. Findings were published in the December 10 online issue of Cancer Cell.
Approximately 160,000 people in the US are diagnosed with NSCLC each year, and roughly 15,000 have metastatic disease with EGFR mutations.
“Multiple methods of resistance to EGFR TKIs have been identified in EGFR-mutant non-small cell lung cancer, but resistance to treatment remains a major challenge,” said Mien-Chie Hung, PhD, chair of Molecular and Cellular Oncology. “Our study identified PKCδ as a common mediator shared by multiple methods of resistance to EGFR TKIs, and it significantly demonstrates inhibition of PKCδ facilitates EGFR TKIs to induce regression of resistant tumors with EGFR mutation.”
EGFR are proteins belonging to a family called receptor tyrosine kinases (RTKs) frequently mutated in NSCLC which cause cellular changes, including enhanced cell growth, tumor formation and metastasis. TKIs interrupt EGFR cell signaling and suppress tumor development. Yet treated tumors eventually develop resistance due to multiple mechanisms known collectively as tumor heterogeneity resistance, which includes additional mutations of EGFR and/or overexpression of other RTKs.
New generations of TKIs targeting specific resistant mechanisms have been developed, which help patients live for several more months, but relapse still occurs and patients eventually are left with no treatment options. To overcome tumor heterogeneity resistance, it is critical to identify a common mediator, which, when blocked, may provide effective treatment, Hung added.
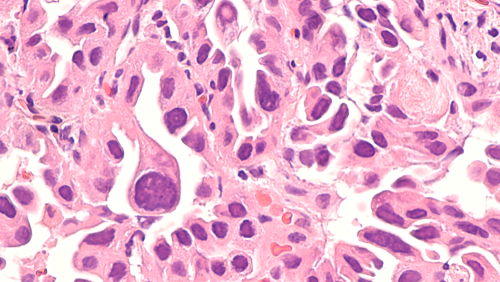
The team observed high levels of PKCδ activation in tumor-bearing mice and patient tissue samples, which revealed PKCδ is a requirement for TKI resistance and is associated with worse progression-free survival following TKI treatment.
The team discovered a combination of two therapies studied in mice, gefitinib and sotrastaurin, appear to be effective as a potential therapy strategy for EGFR-mutant NSCLC TKI resistance. Gefitinib is an FDA-approved TKI for EGFR-mutant NSCLC, while sotrastaurin is approved for use in clinical trials in cancer and other diseases.
“Since gefitinib has received regulatory approval in NSCLC patients and sotrastaurin is available for clinical studies, the combination could be readily tested in clinical trials, especially for patients whose tumor has developed TKI resistance,” said Hung. “It is our hope that new therapies that could result from such studies may be of benefit to patients who have not responded to existing treatments.”
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries