Dapagliflozin as adjunct therapy to insulin may improve glycemic control: DEPICT-2 Study
American Diabetes Association Press Releases Jun 27, 2018
Adding the selective SGLT2 inhibitor dapagliflozin to intensive insulin therapy in adults with type 1 diabetes (T1D) who had suboptimal glycemic control reduced blood glucose levels, aided in weight loss, and led to a reduction in insulin doses, yet also correlated with a slight increase in diabetic ketoacidosis risk compared to placebo, according to the study “Efficacy and Safety of Dapagliflozin in Patients with Inadequately Controlled Type 1 Diabetes—DEPICT-2 Study,” presented yesterday at the American Diabetes Association’s® (ADA’s) 78th Scientific Sessions® at the Orange County Convention Center.
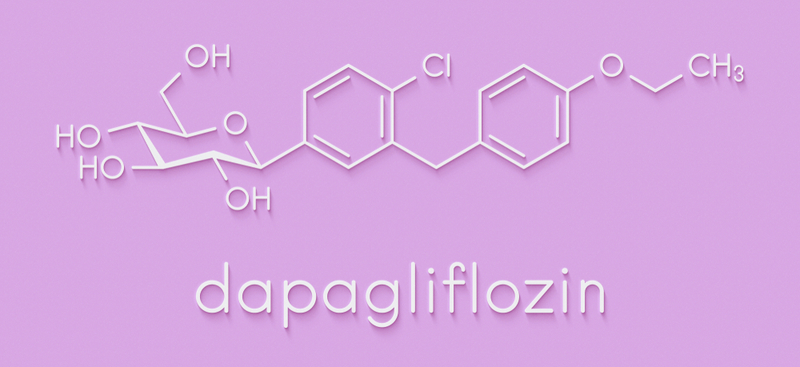
Dapagliflozin is a selective inhibitor of SGLT2—a protein responsible for glucose regulation. SGLT2 inhibitors block the SGLT2 protein involved in glucose reabsorption in the proximal renal tubule of the kidney, which results in an increase in renal glucose excretion and lower blood glucose levels.
DEPICT-2 was a phase 3, double-blind, global study conducted among 137 sites in North America, South America, Europe, and Asia to evaluate the efficacy and safety of dapagliflozin as an add-on to insulin therapy in people with T1D. The trial was similar in design to the DEPICT-1 study, which was published in September 2017.
DEPICT-2 enrolled 813 adults between the ages of 18 and 75 with T1D who had an HbA1c level from 7.5% to 10.5%. Patients were randomly assigned to receive daily, oral doses of either 5 mg of dapagliflozin (271 patients), 10 mg of dapagliflozin (270 patients), or a placebo (272 patients), in addition to their usual insulin, for 52 weeks. The insulin dose could be adjusted by clinicians based on the patient’s self-monitored blood glucose readings, local guidance, and individual circumstances.
This study evaluated patients after 24 weeks on the regimen, and the results showed that compared to placebo, patients treated with 5 mg and 10 mg of dapagliflozin had a decrease in HbA1c levels by .37% to .42%, respectively. The addition of dapagliflozin was also accompanied by weight loss, with the patients on 5 mg losing an average of 3.2% of their body weight, and the patients who received 10 mg losing 3.7% of their body weight, compared to an average weight loss of .02% in the placebo group. There was also a reduction in insulin doses in the dapagliflozin 5-mg and 10-mg group (-10.78% to -11.08%, compared to placebo). Continuous glucose monitoring showed more improved, stable glycemic values among dapagliflozin-treated patients, leading to an increased time-in-range over 24 hours of 2 h 10 min with dapagliflozin 5 mg, and a little over 2 h 30 min with dapagliflozin 10 mg, compared to placebo.
The safety analysis showed no significant increased risk of hypoglycemia, and in particular, severe hypoglycemia among patients treated with dapagliflozin: 17 patients (6.3%) from the dapagliflozin 5-mg group, 23 patients (8.5%) from the dapagliflozin 10-mg group, and 21 patients (7.7%) from the placebo group experienced one or more episodes of severe hypoglycemia over the 24-week period. However, the dapagliflozin patients did have an increased risk of diabetic ketoacidosis (DKA), a known complication for patients with diabetes that affects those with type 1 diabetes more frequently than patients with type 2 diabetes. No patients from the placebo group experienced DKA, compared to 2.6% for the dapagliflozin 5-mg group and 2.2% for the dapagliflozin 10-mg group.
“The results of our study add to a growing body of evidence showing that SGLT2 inhibitors have the potential to serve as promising adjunct therapies in people with T1D who are not consistently in their target blood glucose range,” said Chantal Mathieu, MD, PhD, professor of medicine at the Catholic University of Leuven, Belgium. “Results of the DEPICT-2 study were consistent with those of its twin study, DEPICT-1, which followed mostly European and American patients with T1D. This new study had a greater global reach, with about a quarter of patients being from Asia. The benefits seen in both studies are important to people with T1D. Introduction of dapagliflozin as an adjunct therapy could be an interesting and exciting new treatment for T1D, almost 100 years after the discovery of lifesaving insulin. However, adding dapagliflozin to the insulin regimen needs to be balanced against the increased risk of DKA, and this therapy should be coupled with intensive educational measures to cope with the small, but real risks.”
The study has been accepted for publication and will be featured in its entirety in an upcoming issue of Diabetes Care, the ADA’s peer-reviewed research journal dedicated to diabetes treatment and prevention.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries