Interventions in Recurrent Pregnancy Loss (RPL): Dr. Kiran Guleria
M3 India Newsdesk May 27, 2020
Dr. Kiran Guleria throws light on Recurrent Pregnancy Loss (RPL) which is not just a tragedy to couples seeking parenthood but a clinical challenge to physicians too.
RPL is emotionally traumatic for patients and extremely frustrating for treating doctors as the options for evidence based diagnostics and treatment strategies are limited and not very successful.
Pregnancy loss is defined as a spontaneous demise before foetus reaches viability i.e. from the time of conception until 20/22/24 weeks depending upon the law of the land. This could be after spontaneous conception or assisted reproductive technique (ART), but excludes ectopic and molar pregnancies and implantation failure.
Recurrent Pregnancy Loss (RPL) is defined as three or more consecutive pregnancy losses ( seen in 0.4-1%) as per RCOG guidelines (2011) or two or more failed clinical pregnancies as documented by ultrasonography or histo-pathologic examination as per ASRM guidelines (2013) or loss of two or more pregnancies (2%) as per ESHRE guidelines (2018)
- Primary RPL refers to pregnancy loss in a woman who never carried her pregnancy to viability
- Secondary RPL refers to pegnancy loss in a woman with a previous live birth; it carries a better prognosis
Aetiology
The cause of RPL can fall broadly under the following heads- genetic, thrombophilia, immunological, endocrine, anatomic, and environmental factors.
Two concerns that bother an obstetrician are that cause can be known in 50% of patients only. Secondly, the recurrence risk is modified by the number of previous losses ranging from 10% (previous one loss) to 35% (previous 3 or more losses), cause of previous loss, gestational age and inter-pregnancy interval and maternal age. Risk of pregnancy loss is lowest in 20 to 35 years and rapidly increases after 40 years. Stress is usually associated with RPL, but is not a direct cause of pregnancy loss.
Investigations & interventions in RPL
History: A good medical and family history could be used to tailor diagnostic investigations in RPL. Prognosis can be based on the number of preceding pregnancy losses and the woman's age. Certain prognostic tools based on risk factors can be used to provide an estimate of subsequent chance of live birth in couples with unexplained RPL.
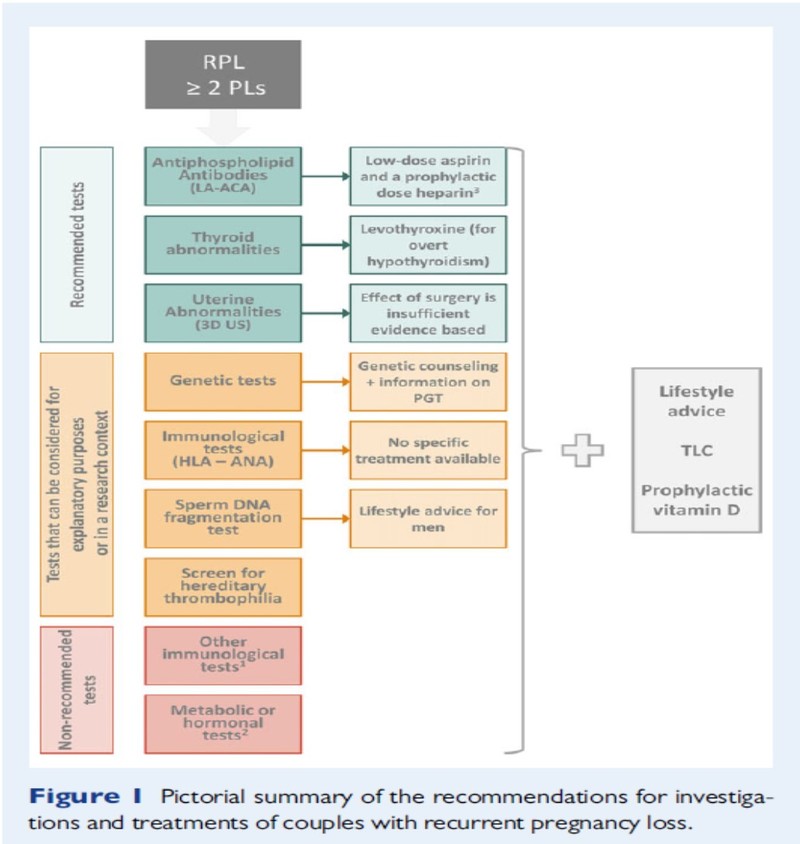
Screening for genetic factors: About 3-5% of couples with RPL have a major chromosomal rearrangement vs. 0.7% in general population; usually a balanced translocation. Genetic analysis of pregnancy tissue is not routinely recommended except for explanatory purposes. If this analysis is needed, an array-based comparative genomic hybridisation (array-CGH) is recommended based on reduced maternal contamination effect. Parental karyotyping is also not routinely recommended in RPL. It can be done after individual assessment of risk. Young age, >3 losses, >2 losses in sibling/parent, unknown stillbirths, abnormal baby are some of the indications for parental karyotype.
Therapeutic interventions for RPL due to genetic/chromosomal causes: To increase chances of subsequent live birth rate, all couples with an abnormal foetal or parental karyotype should receive proper genetic counselling regarding the possible treatment options and their advantages and disadvantages. Pre-implantation genetic testing shows no clear benefit of treatment.
Screening for thrombophilia: There is no recommendation to screen for hereditary thrombophilia unless in research context, or in women with additional risk factors for thrombophilia. But, there is a strong recommendation to screen for antiphospholipid antibodies (LA, ACA- IgG & IgM), after two pregnancy losses. Screening for β2 glycoprotein I antibodies (aβ2GPI) should also be considered after two pregnancy losses.
Therapeutic intervention in the form of antithrombotic: Prophylaxis for RPL in women with hereditary thrombophilia is not used unless for research, or if indicated for VTE prevention.
Antiphospholipid syndrome (APS) & RPL (history of > 3 pregnancy losses) is treated with low dose aspirin (75–100 mg/day), starting before conception, and a prophylactic dose heparin (UFH or LMWH) starting at a positive pregnancy test. Anticoagulant treatment can also be offered to women with two pregnancy losses and APS, mostly in the context of clinical research.
Immunological assessment: HLA determination is not recommended. Only HLA class II determination (HLA-DRB1*15:01 and HLA-DQB1*05:01/05:2) is considered in Scandinavian women with secondary RPL after the birth of a boy, for prognostic purposes. Measurement of anti-HY antibodies, cytokine testing, cytokine polymorphisms, ANA testing (only for explanatory purposes), natural killer (NK) cell testing of either peripheral blood or endometrial tissue and anti-HLA antibodies testing is not recommended.
Screening for metabolic/endocrine abnormality: Thyroid screening (TSH and TPO-antibodies) is strongly recommended. Abnormal TSH and TPO-antibody levels should be followed by thyroxine (T4) testing. However, aassessments of PCOS, fasting insulin and fasting glucose are not recommended. Prolactin testing is also not recommended in the absence of symptoms of hyperprolactinemia (oligo/amenorrhoea). Similarly, we should not order ovarian reserve testing, luteal phase insufficiency testing, androgen testing, LH testing, and measurement of plasma homocysteine and Vitamin D.
Therapeutic intervention in RPL & metabolic or hormonal abnormalities:
- Overt hypothyroidism before conception or during early gestation should be treated with levothyroxine. There is a conflicting evidence regarding treatment of subclinical hypothyroidism and RPL.
- Treatment may reduce the risk of miscarriage. If a woman with subclinical hypothyroidism/thyroid autoimmunity and RPL is pregnant again, TSH level should be checked in early gestation (7–9 weeks) and hypothyroidism should be treated with levothyroxine.
- There is insufficient evidence to treat euthyroid women with thyroid antibodies and RPL outside a clinical trial.
- Use of progesterone to improve live birth rate in luteal phase insufficiency and use of hCG to improve live birth rate in luteal phase insufficiency is advised.
- Supplementation with metformin in pregnancy to prevent pregnancy loss in women with glucose metabolism defects has not been found to be useful and thus not recommended.
- Bromocriptine treatment can be considered in hyperprolactinemia to increase live birth rate. During preconception counselling in these women, it is a good advice to consider prophylactic vitamin D supplementation.
Screening for Anatomical abnormalities: All women with RPL should have an assessment of the uterine anatomy as anatomical abnormalities are seen in 10-50%. Preferred surveillance technique is 3D trans vaginal scan (has high sensitivity and specificity) which can distinguish between septate uterus and bicorporeal/bicornuate uterus with normal cervix. Sonohysterography (SHG) is more accurate than HSG in diagnosing uterine malformations in the absence of 3D ultrasound, or when tubal patency has to be investigated. If a Müllerian uterine malformation is diagnosed, further investigation (including that of the kidneys and urinary tract) should be considered. MRI is not recommended as first-line option, but can be used if 3D ultrasound is not available.
Therapeutic Intervention for RPL and uterine abnormalities
Septate uterus: Whether hysteroscopic septum resection benefits (improving live birth rates, & decreasing miscarriage rates, without doing harm), should be evaluated in the context of surgical trials.
Bicorporeal uterus with normal cervix: Metroplasty is not recommended.
Hemiuterus: Uterine reconstruction is not recommended.
Bicorporeal uterus and double cervix (former AFS- didelphic uterus): Insufficient evidence for metroplasty.
Submucosal fibroids or endometrial polyps: Insufficient evidence for hysteroscopic removal.
Intramural fibroids: Surgical removal not recommended. Insufficient evidence to recommend removing fibroids that distort the uterine cavity.
Intrauterine adhesions: Insufficient evidence for hysteroscopic/surgical removal; and if done, precautions are to be taken to prevent recurrence.
History of second-trimester pregnancy losses & suspected cervical weakness: Offer serial cervical sonographic surveillance.
Pregnancy with h/o recurrent second-trimester pregnancy loss due to cervical weakness: Consider a cerclage; but no evidence that this treatment increases perinatal survival.
Male partner assessment - Does the quality of male gametes matter?
In the male partner, assess lifestyle factors (smoking, alcohol consumption, exercise pattern, and body weight) and suggest desired changes. Assessing sperm DNA fragmentation can be considered for explanatory purposes, based on indirect evidence.
Therapeutic Intervention for male: Sperm selection is not recommended as a treatment in couples with RPL and antioxidants for men have not been shown to improve the chance of a live birth.
Unexplained RPL is seen in almost 50% patients where no cause is identified despite investigations. People have tried various ‘hit and trial’ treatments but many of these therapies are not recommended as these are not backed by evidence. Lymphocyte immunisation which may have serious adverse effects, intravenous immunoglobulin, glucocorticoids, heparin or low dose aspirin are not recommended.
Progesterone is usually prescribed by all, though evidence is lacking. But intralipid therapy, granulocyte colony stimulating factor (G-CSF) and endometrial scratching are of no use. In couples with RPL, irrespective of a cause low dose folic acid is routinely started pre-conceptionally to prevent neural tube defects, but it has not been shown to prevent pregnancy loss in women with unexplained RPL.
Certain health behaviour modifications can reduce the risk of pregnancy loss in women with a history of RPL. Smoking can have a negative impact on chances of a live birth, and cessation of smoking is recommended. Maternal obesity or significant underweight is associated with obstetric complications and can have a negative impact on chances of a live birth and on general health. So these women should strive for healthy normal range BMI. Excessive alcohol consumption is a possible risk factor for pregnancy loss and a proven risk factor for foetal problems (foetal alcohol syndrome), so limit alcohol consumption.
Organization of care for RPL
Such women/couples should be cared for in a dedicated RPL clinic, where all their medical and psychosocial needs are addressed under the same roof. But it must be made clear to them that investigations do not necessarily lead to treatment options. These clinics should have experienced staff members with appropriate listening and counselling skills and appropriate imaging facilities should be made available.
To conclude, we must individualise investigations and treatment for RPL appropriate to each woman or couple, based on age, fertility/sub-fertility, pregnancy history, family history, previous investigations and/or treatments.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Kiran Guleria is the Director-Professor at Department of Obstetrics & Gynecology, University College of Medical Sciences & GTB Hospital, Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries