Anti-TB drugs can add to the risk of TB re-infection
ANI Mar 27, 2019
A recent study revealed that treatments available for tuberculosis (TB) caused by Mycobacterium tuberculosis (Mtb), may not always prevent re-infection.
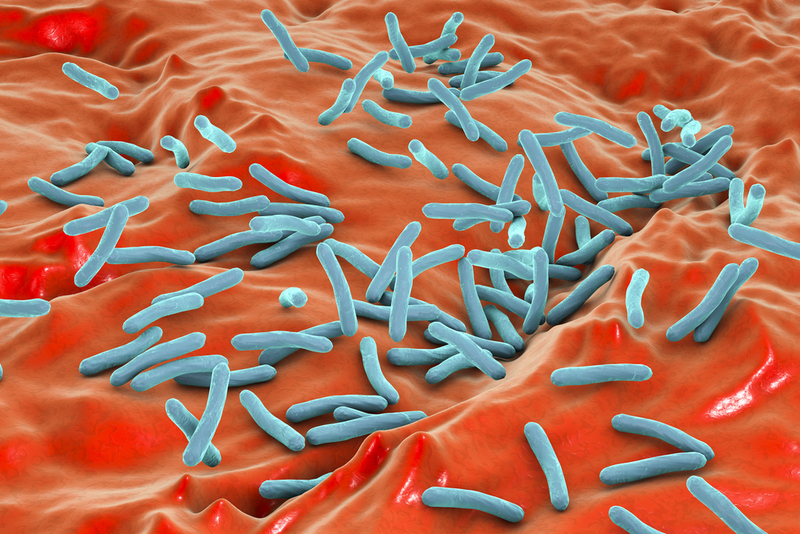
In a recent study published in the Journal of Mucosal Immunology, researchers have shown that anti-TB drugs caused changes to gut microbiota, the diverse community of microbes living in human beings’ intestines, and increased susceptibility to Mtb infection. According to the study, “gut microbiota are critical to keep us healthy; digest food, combat pathogenic microbes and reinforce our immune system. Recent research has shown that chronic use of antibiotic leads to disruption of this community, which can in turn lead to dysregulation of the immune system.”
However, it remains unclear if changes in the composition of the microbes living in our gut have an influence on TB infection.
A team of researchers found out the impact of anti-TB drugs on microbiome by treating mice with the most commonly used anti-TB drugs, isoniazid, rifampicin and pyrazinamide, for a period of eight weeks.
They found that while all three drugs significantly altered the composition of the mice's gut microbiome, but mice treated with isoniazid combined with pyrazinamide showed an increase in susceptibility to Mtb infection. To make sure the vulnerability of the host to Mtb infection was due to a compromised gut microbiota, the researchers looked at faeces. By transplanting faeces from mice that had been treated with anti-TB drugs (specifically isoniazid and pyrazinamide) into untreated mice prior to infection, they were able to show for the first time that faecal transplant was sufficient to compromise immunity to Mtb.
Dr. Irah King, Meakins Laboratories, Research Institute of the McGill University Health Centre (RI-MUHC), and his colleagues also wanted to better understand the gut-lung axis, a bi-directional communication system between micro-organisms residing in the gastrointestinal tract and the lungs, in order to know how this might be involved in Mtb infection and immunity.
To do so, they evaluated a number of lung cell types known to be important for resistance to Mtb infection. Following anti-TB treatment, alveolar macrophages, a type of immune cell located in the airways of mice and humans and the first cell to encounter Mtb upon infection, were compromised in their ability to kill Mtb.
"We need to do more research in order to understand how the microbiome affects alveolar macrophages because these cells are critical for controlling early TB infection. We also need to identify the molecular pathways involved in the gut-lung axis,'' explained King.
"Anti-TB therapies have been incredibly efficient in controlling the TB epidemic by decreasing morbidity and mortality associated with Mtb. Now, this work provides a basis for novel therapeutic strategies exploiting the gut-lung axis in Mtb infection,'' said King.
Researchers are already thinking of monitoring patients who are being treated with these drugs to see how their gut microbiota changes over time once the treatment has stopped. The idea will be to control changes to the microbiome in combination with drugs that are effective at killing Mtb.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries