Time-in-range: Do not miss out on this new metric in diabetes: Dr. Jothydev Kesavadev
M3 India Newsdesk Aug 23, 2020
Dr. Jothydev Kesavadev writes on glucose monitoring in diabetes and the significance of time-in-range as a new metric for better glycaemic control in patients with diabetes.
For our comprehensive coverage and latest updates on COVID-19 click here.

Glucose monitoring in diabetes started with Dr. Benedict’s introduction of urine glucose testing in 1908. For more than half a century, that was the only methodology available for monitoring diabetes. Later, blood glucose monitoring with glucose meters and continuous glucose monitoring became popular. With rapid developments in the technology, CGM devices became more and more accurate with a possible threat to even the existence of glucose meters. The biggest advantage of continuous glucose monitoring is the availability of comprehensive glucose data measured once in 5-15 minutes (depending on the device) over a period of 7-14 days. On the contrary, the widespread adoption of CGM was hindered by difficulties in interpreting the dense data which could rob away several minutes of a consultation.
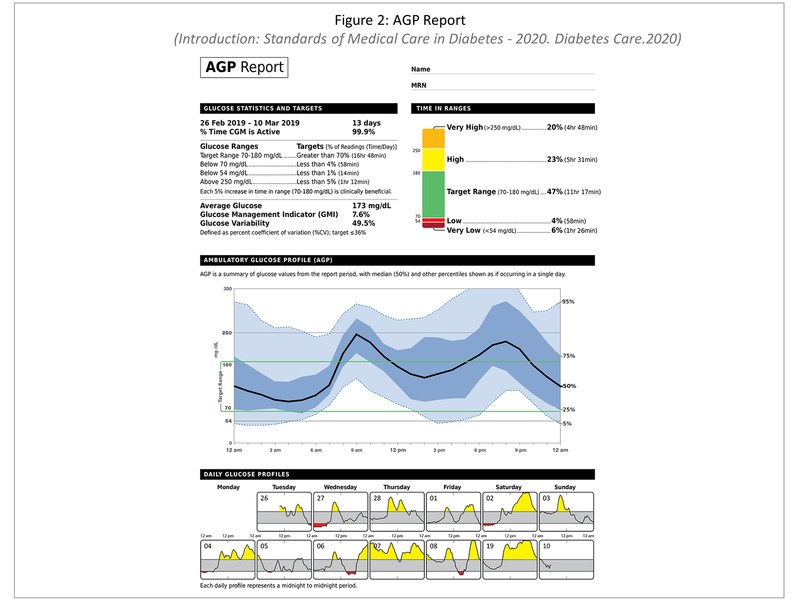
The introduction of time in range as the new glucose metric for the easy interpretation with the aid of AGP report (Ambulatory Glucose Profile) is considered a landmark event in diabetology.
AGP originally developed by Dr.Roger Mazze in 1987 and currently owned by International Diabetes Centre, Minneapolis is meant for uniform reporting of blood glucose data so that the entire glucose data is collapsed to look like a model single day graph. AGP report and time in range was adopted by American Diabetes Association (ADA) in 2019 and are now included in the ADA 2020 clinical practice guidelines.
HbA1c fails to capture the data on glucose directions, the amplitude of glucose excursions, hypoglycaemic events, duration spent in hyper, hypo etc. Moreover, A1c could be wrong in conditions such as anaemia, thalassemia, pregnancy and chronic kidney disease (CKD) etc. [1] Two subjects with the same A1c level will have 2 different patterns in CGM which is regarded to be clinically significant in terms of glucose variability. For instance, in a landmark JDRF CGM study, people with diabetes whose A1c levels were <7% spent more than 90 minutes/day with glucose levels <70 mg/dL. [2]
The 2019 International consensus conference organised by the ATTD had identified “Time-in-range” (TIR) as a new metric for better glycaemic control in subjects with diabetes. [3] The acceptance of TIR by the ADA as a metric for glycaemic control beyond HbA1c was on the grounds of evidence-based clinical studies done by various diabetes research groups. Beck et al. did a study where they capitalised on the glucose values captured seven times once every 3 months during the course of the six plus years of the Diabetes Control and Complications Trial (DCCT). The study revealed that with each 10% drop in TIR, there was an increase in the risk of retinopathy by 64% and of microalbuminuria by 40%. [4]
Dr. Vigersky, McMohan, Beck et al, Kesavadev et al have reported a time in range of above 70% correlated with an A1c of 7%. Every 10% increase in the time in range result in 0.5-0.8% reduction in A1c and thereby significant reduction in the complications of diabetes. [4-7]
Time-in-range
TIR is defined as the percentage of time an individual spends with their blood glucose levels in the target range. Time in Range includes three key CGM measurements: time spent within target glucose range (TIR), time spent below target glucose range (TBR), and time spent above target glucose range (TAR) in a duration of 24 hours. For instance, if a person's TIR is 50%, the person spends 12 hours within the target glycaemic range. TIR detection is possible with blood glucose meters also. Currently, the TIR reports are directly obtainable from Libre/Libre Pro and Dexcom CGM devices. In the near future, all the CGM devices will have the capability of generating AGP report. [1, 6]
Time-in-range goals
The International consensus recommends a target range between 70-180 mg/dL for individuals with low risk type 1 diabetes and type 2 diabetes, and 63-140 mg/dL in pregnant type 1 diabetes, along with a set of targets for the time per day [% of CGM readings or minutes/hours].
TIR simplifies the crux of these values like that; a patient with diabetes should aim to spend at least 16 hours, 48 minutes a day or more than 70% of their time in the blood glucose range of 70-180 mg/dL. The recommendations also outline fixing targets for people with diabetes who are older and/or considered high-risk and the time-in-range bar was set at 50% for these category. [3] It is the functional age and not the chronological age which needs to be considered since hypoglycaemia will pose a high risk in the presence of co-morbidities.
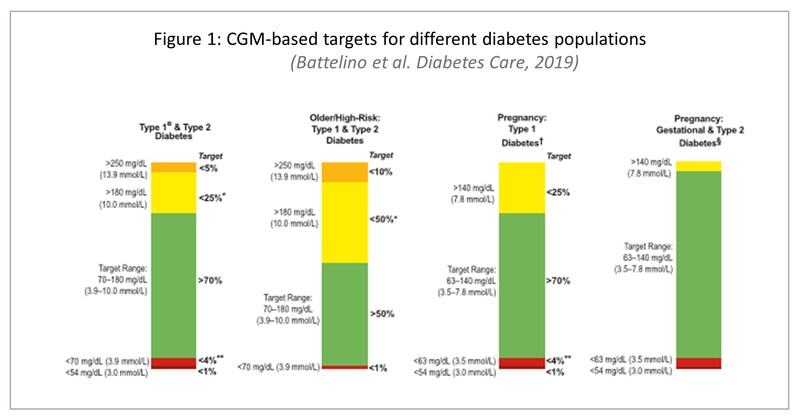
Associated with the term 'Time-in-range', are the two terminologies 'Time-above-range' which represents the time a person spent above the accepted range and 'Time-below-range' which represents the time a person spent below the range (Figure 1).
According to the new guidelines, for patients with diabetes, the time spent below 70 mg/dL should be less than 1 hour a day or under 4% of the time and time spent at or above 180 mg/dL should be less than 6 hours a day or 25% of the time. For people with serious hypoglycaemia, the time spent below 54 mg/dL should be less than 15 minutes a day or 1% of the time and the time spent above 250 mg/dL should be less than 1 hour and 15 minutes a day or 5% of the time. [3]
Significance of TIR
The AGP report (Figure 2) as recommended by the ADA has incorporated 10 glucose metrics along with the normal TIR ranges, in the handout to the patient. Compared to a detailed CGM report, this simplifies the datasets into actionable information. At a glance, the physician, the diabetes educator and the patient will have an overall impression on the necessity to change the behaviors, therapy, identify the areas with a high risk of hypoglycaemia, the necessity to reduce the glucose exposure, reduce the variability including both intra-day and inter-day. Most recent studies are supporting time in range emerging as a hard endpoint in clinical trials and very soon, in clinical practice.
This article was originally published on May 13, 2020.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Jothydev Kesavadev is an acclaimed Diabetologist, and Chariman and Managing Director at Jothydev's Diabetes Research Centre, Kerala.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries