Thyroid Interpretation and Management During Pregnancy
M3 India Newsdesk Aug 30, 2023
This article comprehensively discusses the diagnosis and treatment of thyroid disorders during pregnancy. It also outlines key recommendations from different medical societies regarding screening, management, and interpretation of thyroid function during pregnancy.
Thyroid disorders during pregnancy are commonly encountered by gynaecologists and primary care physicians in their day-to-day practice.
Pregnancy thyroid disorder consists of:
- Hypothyroidism
- Subclinical hypothyroidism
- Hyperthytroidism
- Hyperemesis gravidarum
- Thyroid nodule
- Postpartum thyroiditis
Subclinical hypothyroidism is the most common thyroid disorder in pregnancy. Due to complex hormonal changes during pregnancy thyroxine requirements are higher as compared to non-pregnant females.
The treatment of thyroid disorders during pregnancy ensures a safe pregnancy with minimal maternal and neonatal complications.
This article highlights the key recommendations by various societies for the treatment of thyroid disorders in pregnancy.
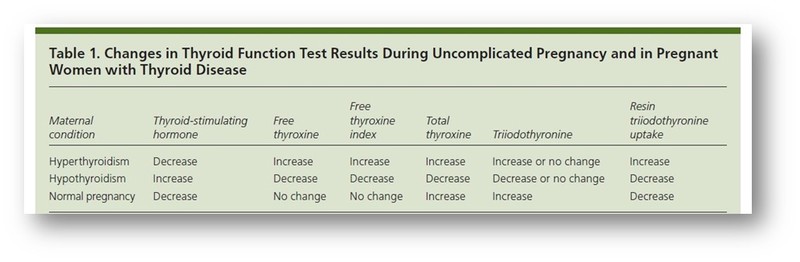 Thyroid Function Interpretation During Pregnancy
Thyroid Function Interpretation During Pregnancy
Screening of thyroid disorder during pregnancy
- As per recommendations by various societies, all pregnant females should be screened at 1st antenatal visit by measuring TSH levels.
- The anti-TPO antibodies should be considered in high-risk groups like females having a personal history of thyroid or other autoimmune disorders, women with goitre, a history of miscarriage or preterm delivery, or women with type 1 DM.
- In the case of positive Anti-TPO antibodies and normal TSH, there is no evidence for administering LT4 therapy or corticosteroids.
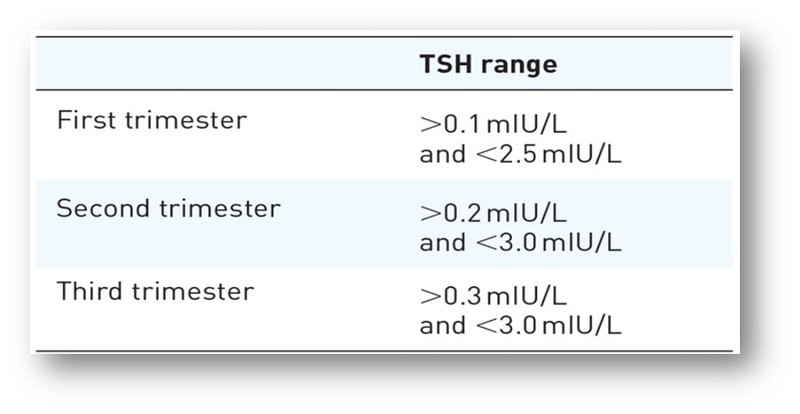
Trimester-specific ranges for TSH levels
Management of hypothyroidism
- Overt hypothyroidism is associated with serious adverse effects on the fetus. Therefore hypothyroidism should be treated as per guidelines.
- Subclinical hypothyroidism which is defined by serum TSH above the upper limit of the trimester-specific reference range with normal T4 should be treated with levothyroxine (LT4) as SCH may be associated with adverse outcomes for both the mother and offspring.
- The LT4 dose usually needs to be incremented by 4 to 6 weeks gestation and may require a 30% or more increase in the dosage.
- If overt hypothyroidism is diagnosed during pregnancy, the LT4 dose (1.6-2.0 μg /kg/d) should be titrated rapidly to reach the desired trimester-specific TSH ranges. TFT should be measured within 30-40 days and then every 4-6 weeks.
- After delivery most hypothyroid women need to decrease the LT4 dose received during pregnancy to the pre-pregnancy dose.
- Women with thyroid immunity who are euthyroid in the early stages of pregnancy are at higher risk of developing hypothyroidism and therefore should be monitored with TSH every trimester.
Maternal Hyperthyroidism: Maternal aspect
- If a subnormal serum TSH concentration is detected during gestation, hyperthyroidism must be distinguished from both normal physiology of pregnancy and gestational thyrotoxicosis because of the adverse effects of overt hyperthyroidism on the mother and fetus.
- Differentiation of Graves’ disease from gestational thyrotoxicosis is supported by the presence of clinical evidence of autoimmunity, typical goitre, and presence of TSH receptor antibodies (TRAb). TPO-Ab may be present in either case.
- The presence of subclinical hyperthyroidism during pregnancy does not warrant any treatment, as there is no evidence that treatment will improve pregnancy outcomes.
- Overt hyperthyroidism should be treated with propylthiouracil (PTU) in the first trimester and with methimazole (MMI) 2nd trimester onwards. MMI may be considered in patients not tolerating PTU or having an adverse response to PTU. 10mg MMI is considered equal to 100-150 mg of PTU.
- Long-term use of beta-blockers is associated with adverse effects; hence they are recommended only for the symptomatic control of thyrotoxicosis or while awaiting response to the anti-thyroid medication or surgery. Propanolol (40-120mg/day in divided doses) is the most common beta-blocker used.
- In case of pregnancy after a previous ablative therapy for hyperthyroidism, reassessment of TRAb level at the beginning of the pregnancy should be checked to determine the chance of fetal or post-natal hyper or hypothyroidism.
- Subtotal thyroidectomy may be indicated during pregnancy (usually during 2nd trimester) as therapy for Graves’s Disease if:
- The patient has a severe adverse reaction to ATD therapy;
- Persistently high doses of ATD are required (over 30 mg/d of MMI or 450 mg/d of PTU)
- The patient is non-adherent to ATD therapy and has uncontrolled hyperthyroidism.
Maternal Hyperthyroidism: Fetal aspect
- Thyroid receptor antibodies can freely cross the placenta stimulate the fetal thyroid and cause fetal thyrotoxicosis. These antibodies should be measured in the mother with
- Current Graves’ disease
- A history of Graves’ disease and treatment with 131I or thyroidectomy before pregnancy
- A previous neonate with Graves’ disease
- A previously elevated TRAb
- Women who have a negative TRAb and do not require ATD have a very low risk of fetal or neonatal thyroid dysfunction.
- Iodide should not be given to the pregnant female as it can lead to fetal goitre.
- The use of Iodine 131 is contraindicated during pregnancy because of the possible teratogenic effect of radiation.
- If the mother is euthyroid but positive for TRAb, there is a possibility of fetal thyrotoxicosis which should be assessed by FHR (>160bpm). If all other causes of fetal tachycardia have been ruled out, start the mother on methimazole/ carbimazole to control fetal thyrotoxicosis and LT4 to maintain maternal euthyroidism.
- Once fetal hyperthyroidism is diagnosed, the treating physician should start ATD therapy for the mother. The fetus should be re-evaluated for clinical improvement by USG in 2 weeks and appropriate when dose adjustment is done.
Thyroid nodules in pregnancy
- A palpable thyroid nodule should be evaluated by measuring serum TSH and a USG assessment of the thyroid gland followed by FNAC if required.
- If the nodule is benign, no further evaluation is needed, except in the cases with increased TSH, where the LT4 should be given to normalise TSH.
- If the nodule turns out to be malignant or shows rapid growth surgery should be considered in 2nd trimester.
- Post surgically patients should be maintained LT4 therapy with monitoring of TSH and free T4 levels every 6 weeks.
- Postsurgical Iodine-131 whole-body scintigraphy and radioiodine remnant ablation are contraindicated during pregnancy and lactation.
Postpartum thyroiditis
Postpartum thyroiditis is defined as thyroid dysfunction within 12 months of delivery that can include clinical evidence of hyperthyroidism, hypothyroidism or both hyperthyroidism followed by hypothyroidism.
- There is insufficient data to recommend screening of all women for postpartum thyroiditis. Prevalence of PPT in women with type 1 Diabetes, Grave’s disease in remission and chronic viral hepatitis is greater than in the normal population, screening by TSH is recommended at 3 and 6 months postpartum.
- Thyroid function in most of the cases with postpartum thyroiditis returns to a normal state within 12 to 18 months of the onset of symptoms.
- The majority of women in the hyperthyroid phase with symptoms like fatigue, irritability, weight loss, palpitations or heat intolerance do not require active intervention with ATD, such symptomatic cases should be managed with a short course of beta blockers preferably propanolol.
- Postpartum thyroiditis may give rise to hyperthyroid symptoms of fatigue, irritability, weight loss, palpitations or heat intolerance
- The thyrotoxic phase usually lasts only a few months and affected women often are only mildly symptomatic
- The duration of therapy with LT4 should be approximately 1 year postpartum or until the woman completes her family. No clear association between the presence of PPT or thyroid antibodies and postpartum depression has been established.
- Women with postpartum depression should be screened for hypothyroidism and appropriately treated.
Gestational hyperemesis and hyperthyroidism
- Many women with hyperemesis gravidarum have abnormally high serum T4 levels and low TSH levels, these thyroid function abnormalities result from the TSH receptor stimulation from high concentration of beta HCG.
- TFT should be done in all patients with hyperemesis gravidarum as such patients are at risk of developing transient hyperthyroidism.
- This condition is usually self-limiting with most patients requiring symptomatic treatment and does not require anti-thyroid treatment. It can be differentiated from intrinsic thyroid disease on the basis of the absence of typical symptoms and signs of hyperthyroidism, absence of goitre and thyroid antibodies.
Autoimmune thyroid disease if pregnancy
Currently, routine screening and treatment of autoimmune thyroid disease in euthyroid pregnant women is not warranted.
Points to ponder on
- World Health Organization has revised the reference of Median Urinary Iodine (MUI) for adequate iodine nutrition in pregnancy from 150 to 250 μg/L and the Recommended Dietary
- Allowance (RDA) for iodine in pregnancy from 200 to 250 μg/L. The thyroid profile interpretation and timely management are essential in managing thyroid disorders in pregnancy.
- Patients must be referred to an endocrinologist for management of thyroid disorders in pregnancy to avoid the complications associated with them.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist, physician and an obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries