Summary of the 2017 ESCMID-ECMM-ERS Guideline for Aspergillus diseases
M3 India Newsdesk Jul 27, 2018
At an estimated 200,000 cases being reported every year, Aspergillus diseases have become significant contributors to mortality in patients with hematological malignancies and transplant recipients. To tackle and manage the disease effectively, experts from four European societies recently collaborated and published the 2017 ESCMID-ECMM-ERS guidelines.
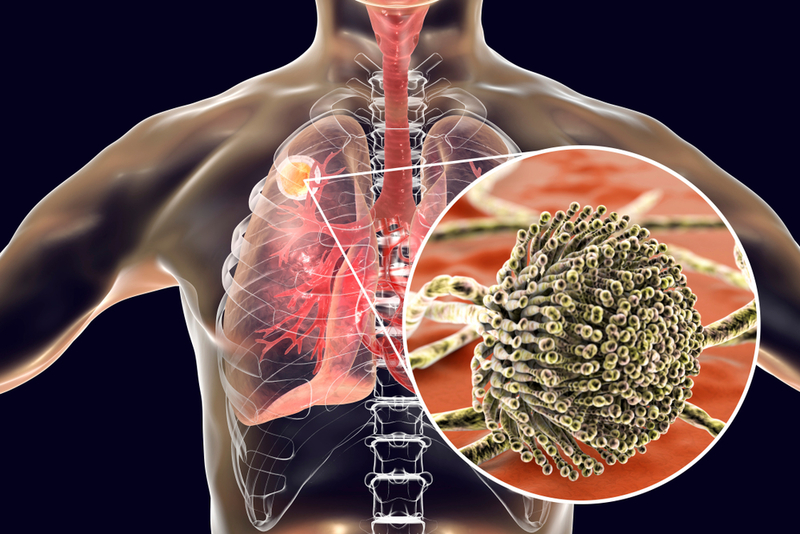
The new guidelines discuss diagnostic procedures, imaging, microscopy, antifungal testing, treatment strategies, secondary prophylaxis, and treating children with Aspergillus diseases. Some of the key points of the guideline pertaining to focus areas of the disease like diagnosis, management, and prophylaxis have been summarized below.
Diagnosis
A diagnosis for Aspergillus disease should be made after gathering all clinical, radiological, and microbiological data.
- For patients presenting with suspected invasive pulmonary aspergillosis (IA), it is recommended to perform a chest computed tomography and bronchoscopy with bronchoalveolar lavage (BAL). Pulmonary CT angiography can be considered for early diagnosis, and for MRI for patients where CT is not a feasible option.
- Microscopy and culture should not be missed while trying to arrive at a diagnosis. Direct microscopy technique, ideally with the use of optical brighteners, is strongly recommended for invasive aspergillosis. Since sensitivity of this technique would only be around 50%, cultures using respiratory secretions also need to be prepared from untreated sputum and centrifuged BAL fluid.
- Non-culture-based assays are also recommended, as they have higher sensitivity than culture-based tests for diagnosis. Galactomannan (GM) can be detected in BAL and is reported as optical density index (ODI). It is a reliable predictor and has good sensitivity, providing diagnostic values for patients undergoing lung transplantation as well.
- Performing a polymerase chain reaction (PCR) test along with the other diagnostic tests, especially GM test enables specific detection. The PCR tests can be used for both blood and BAL, and the combination with biomarkers for both tests leads to a more accurate diagnosis.
- Molecular detection is strongly recommended for hyphael-positive biopsy samples. However, antibody detection is not necessary for diagnosis of IA.
- Anti-fungal susceptibility testing is suggested in patients with invasive disease, excluding the azole-naive patients, in the regions where resistance has been detected. Since resistance is so rampant, Aspergillus isolates must be identified at the complex species level because individual colonies from a single specimen can show variations in anti-fungal resistance.
Treatment
- Isavuconazole and voriconazole are the most preferred agents for first-line treatment of invasive aspergillosis. Combination of antifungals is usually not recommended as primary treatment.
- Use of liposomal amphotericin B or amphotericin B lipid complex is recommended for species with high azole MICs. Micafungin can also be considered is these cases.
- In case of environmental azole resistance, first-line therapy with voriconazole plus echinocandin or liposomal amphotericin B should only be initiated if azole resistance rates are higher than 10%.
- Therapeutic drug monitoring is strongly advised in patients being treated with posaconazole suspension or voriconazole (in any form) for invasive aspergillosis and in refractory disease cases.
Paediatric patient considerations
- Therapeutic drug monitoring is again recommended for children who are on mould-active azoles for prophylaxis or treatment.
- Voriconazole can be used as first-line treatment in all paediatric patients with IA, except neonates, where Liposomal amphotericin B should be the first choice.
- Diagnosis of pulmonary IA should be followed by investigation of other sites, especially the CNS for spread of infection.
- Salvage therapy and breakthrough infections would require a different class of antifungals.
- Primary antifungal prophylaxis should be considered for high risk patients (recurrent leukemia- AML and ALL, bone marrow failure syndrome with neutropenia, allogenic HSCT recipients, chronic granulomatous disease, and lung transplant recipients) who are at threat for developing invasive aspergillosis.
- Secondary prophylaxis is necessary if risk factors persist, so as to prevent recurrence but antifungal treatment should be targeted at the Aspergillus species that caused the first occurrence.
The above points are the key takeaways of the comprehensive ESCMID-ECMM-ERS guideline and are recommended to be used in the clinical setting when dealing with Aspergillus diseases, especially Invasive Aspergillosis (IA) and Chronic Pulmonary Aspergillosis (CPA). The expert groups do plan to publish more material in support of these recommendations in the near future.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries