Recognising and Managing Ocular Emergencies
M3 India Newsdesk Sep 26, 2024
This article explains common ocular emergencies such as Central Retinal Artery Occlusion, chemical injuries, open globe injuries, and macula-on retinal detachment. It also emphasises the need for immediate medical intervention to prevent permanent vision loss.
Central Retinal Artery Occlusion (CRAO)
1. CRAO is an ophthalmic and medical emergency. Prompt referral to a stroke clinic is necessary to minimise the risk of secondary ischemic events such as cerebral or myocardial infarction.[1]
2. The central retinal artery (CRA) (the first branch of the ophthalmic artery), supplies blood to the inner layers of the retina. Its obstruction may be caused by an embolus causing occlusion or thrombus formation (most common), vasculitis causing retinal vasculature inflammation, traumatic vessel wall damage, or spasm.
3. Common Risk Factors of CRAO are:
- Older age
- Male gender
- Smoking
- Hypertension
- Diabetes
- Dyslipidemia
- Cardiovascular disease
- Obesity
- Giant cell arteritis [2]
4. Patients present with sudden, painless, monocular vision loss that occurs over seconds. Visual loss may be preceded by episode(s) of transient loss of vision (amaurosis fugax) in the case of embolic sources.
5. As the CRA supplies the inner retina, its occlusion results in ischemia and thus the damage of the inner retina. It first becomes edematous/whitened (opacification of retinal nerve fibre layer) with the classic finding of “cherry red spot” 3 and over time, as the oedema resolves, the inner retina atrophies. The retinal blood vessels show segmental blood flow, described as “box carrying” [3]
6. Rarely an embolus may be seen within the affected blood vessel. Chronic signs of CRAO include pale optic disc, thinned retinal tissue, attenuated vessels and retinal pigment epithelial mottling. It is recommended to undertake an embolic workup on older patients.
7. Evaluation of the heart with echocardiography and a carotid Doppler to look for carotid artery stenosis should be done. A high index of suspicion for Giant Cell Arteritis (GCA) should be kept in cases of sudden vision loss in patients older than 50 years of age with symptoms of GCA, and an erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and complete blood count (CBC) with platelets should be obtained in them. Urgent systemic steroids are needed in such cases to preserve vision in the affected eye and prevent vision loss in the unaffected eye.[4]
8. In young patients presenting with CRAO, vasculitis (inflammatory/ autoimmune) and/or hypercoagulable workup should be performed.
In the event of a retinal artery closure, urgent systemic examination for cerebral vascular accident (CVA) is necessary.
Older patients with acute CRAO should be referred to a stroke centre for further immediate management.
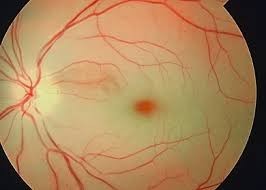
Central Retinal Artery Occlusion- note the diffuse whitening of the central retina with a “Cherry Red Spot” visible in the centre.
Chemical (alkali and acid) injury of the conjunctiva and cornea
Chemical injury of the cornea is a true ocular emergency and requires immediate intervention, as these can produce extensive damage to the ocular surface and anterior segment leading to visual impairment and disfigurement.
Alkali agents are lipophilic and therefore penetrate tissues more rapidly than acids,[5] and are thus generally more harmful than acids. Acids cause damage by denaturing proteins in the tissues. The coagulated proteins act as a barrier to prevent further penetration (unlike alkali injuries).[6]
Treatment
- Protective eye shields are required when handling potentially corrosive substances because most injuries happen at work.
- The first step in treating chemical burns is to remove the offending substance right away and irrigate the injured eye.
- Reducing the amount of time the chemical is exposed to the eye requires irrigation.
- Although a sterile irrigating fluid is preferable, irrigation should be immediately done with any non-toxic liquid including tap water, and should be continued for a minimum of 20-30 minutes. [7]
- Patients with mild to moderate injury have a good prognosis and can often be treated successfully with medical treatment alone.
- Medical treatment aims to enhance recovery of the cornea, augment collagen synthesis, minimise collagen breakdown and control inflammation.
- A broad-spectrum antibiotic drop such as moxifloxacin to prevent superinfection, a cycloplegic agent like atropine and a preservative-free artificial tear drop to comfort the eye, and a steroid drop like prednisolone to help inflammation should be started at the earliest.
- More severe burns necessitate more intensive medical therapies (including oral doxycycline, and Vitamin C), and surgery (debridement of necrotic epithelium, amniotic membrane transplantation).[8],[9]
- Severe burns can lead to complications like glaucoma, dry eyes, scarring of the conjunctiva, and damage to the lids, and all these warrant separate attention.
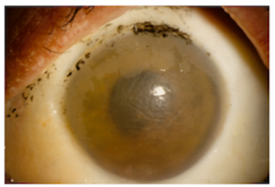
Picture of a severe alkali burn. There is damage and ischemia of the conjunctival blood vessels causing the whitening around the cornea- “limbal ischemia”. Note the loss of transparency in the cornea and loss of lashes.
Open globe injury
- Penetrating and perforating injuries to the eye (open globe injuries) can result in severe vision loss/loss of the eye. Penetrating injuries (no exit wound) are caused by a sharp object that penetrates the eye (full-thickness wound of cornea and/or sclera) but not through and through.
- Perforating injuries (also full thickness), on the other hand, go 'through and through' and therefore have both entrance and exit wounds. These injuries can be due to any sharp (stick, knife, scissors, screwdriver, nail etc) or high-velocity object.
- If one of these objects becomes lodged in the eye, it is referred to as an intraocular foreign body (IOFB), which is seen in around 40% of these injuries.10 Most individuals sustaining eye injuries are males (more workplace accidents) with failure to wear adequate eye protection while performing high-risk activities like basketball and use of tools in homes.
- Patients with open globe injuries usually complain of pain, vision loss, or double vision. In more subtle injuries, there may be minor symptoms such as foreign body sensation, blurred vision, severe redness and light sensitivity.
Signs in a patient with ocular trauma :
- Subconjunctival haemorrhage
- Corneal/ scleral discontinuity
- Irregular anterior chamber depth
- Hyphema
- Peaking of pupil
- Iris deformities
- Uveal prolapse
- Lens disruption
- Posterior segment findings like vitreous haemorrhage
- Retinal tears
Ocular examination after severe trauma can be difficult. Visual acuity and pupillary reflexes assessment are the most important elements of examination. Avoid using techniques that put pressure on the globe that could cause the intraocular contents to extrude, such as B Scan and intraocular pressure monitoring.[11]
In suspected cases of IOFB, computed tomography (CT) scans of the orbits are indicated in cases of poor visualisation of the vitreous and retina. Magnetic resonance imaging (MRI) is contraindicated in such cases.

Picture showing perilimbal corneal perforation with the peaking of the pupil with iris tissue prolapse with surrounding subconjunctival haemorrhage.

Fundus photo showing retained IOFB, impacted in the retina.
When feasible, it is imperative to do surgical exploration and globe repair as soon as possible after the injury, as this has been demonstrated to have a reduced risk of endophthalmitis than delayed repair.[12] [13] Prophylaxis with systemic, topical, and/or intravitreal broad-spectrum antibiotics, should be given and tetanus vaccination should be updated.
Any subsequent procedures like secondary intraocular lens implantation and pars plana vitrectomy, are performed at a later date when the eye is stable. Sympathetic ophthalmia, a rare but serious vision-threatening disease, is a bilateral diffuse granulomatous uveitis that often follows ocular trauma due to a violation of the eye's immune privilege.[14]
Macula-on-rhegmatogenous retinal detachment
Rhegmatogenous Retinal Detachment (RRD) is defined as the separation of the neurosensory retina from the retinal pigment epithelium (RPE) secondary to a ‘rhegma’(break). The fovea, located in the middle 1.5 mm and responsible for central vision, is located in the macula, the central 5.5 mm circular area inside the temporal vascular arcades.
Macula-on- or fovea-sparing RRD indicates that subretinal fluid (SRF) has not involved the macula and thus has not affected central vision. (visual acuity is usually normal in these cases) SRF under the macula indicates some damage despite reattachment. Thus, there is a higher probability of achieving better visual outcomes in macula-on RRD, [15] if operated early.
The symptoms of RRD include flashes, floaters, and a curtain-like shadow over the field of vision. Depending on the extent of retinal detachment and location of retinal breaks, management includes laser barrage/ delimiting laser photocoagulation, pneumatic retinopexy, scleral buckling surgery, or pars plana vitrectomy.
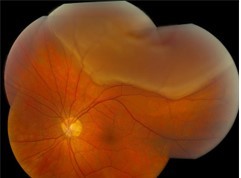
Fundus picture showing a superior “macula-on-RRD”, with superior break. Such a retinal detachment warrants urgent surgical intervention, and an attempt should be made to prevent SRF from reaching the macula intraoperatively.
There could be other eye emergencies that need immediate attention such as ischemic optic neuropathy, endophthalmitis, acute congestive glaucoma, orbital cellulitis, etc, but these are not considered “true eye emergencies” since they don't require immediate medical attention. These conditions, warrant an early management, but not urgent, and are thus not a scope of this article.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Charu Malik is MS, DNB, FNB- vitreoretinal surgery, is an Assistant Professor of Ophthalmology and VitreoRetina and Consultant at SMS&R, Sharda Hospital, Sharda University, G. Noida, and Consultant Ophthalmology at Jaypee Hospital, Noida.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries