Predicting Early Decompensation in Cirrhosis Patients
M3 India Newsdesk Aug 15, 2023
The EPOD score is a new measure for predicting the progression of cirrhosis from asymptomatic to a symptomatic disease state (decompensation). This article explains the need and importance of this EPOD score in the management of cirrhosis patients.
EPOD score- Early Prediction Of Decompensation score
- It’s a new score for the prediction of cirrhosis progression from a symptom-free to a symptomatic disease state that is called decompensation.
- Calculated from three routinely measured blood parameters.
- EPOD score correctly identified low-and high-risk patients.
- Estimated the probability of decompensation within the next 3 years.
- The EPOD score and the predicted 3-year risk of decompensation can be calculated for scientific discussion using the EPOD score calculator.
What is the problem?
- Cirrhosis is a growing global health burden and a major cause of death worldwide.
- It is defined as the end-stage of chronic fibrotic remodelling, which may be caused by continuous liver injury due to chronic alcohol abuse, non-alcoholic fatty liver disease or viral hepatitis.
- In the clinical routine differentiating between patients with compensated or decompensated, cirrhosis is highly relevant as this status critically predicts prognosis.
- Decompensation of cirrhosis is defined by the presence of variceal bleeding, encephalopathy, ascites, hepato-renal syndrome (HRS) and/or jaundice.
- Phase transition of patients with cirrhosis from a compensated to a decompensated state is estimated to occur at rates of 5–7% per year.
- The risk of mortality strongly increases when a patient shifts to the state of decompensated cirrhosis.
- Therefore, predicting the risk of decompensation in a patient with cirrhosis has major clinical implications.
- Moreover, there is an ongoing debate about whether well-known prognostic indicators of survival such as the MELD-Score or Child-Pugh Score may predict survival less accurately in compensated cirrhosis.
- At present, clinical scores were mainly established to calculate the risk of death in patients with cirrhosis.
- To improve the surveillance strategy of patients with cirrhosis such a score that defines the risk of phase transition—compensated versus decompensated state—would have major advantages.
Why Its important to develop a new score?
- It is a critical step of phase transition in patients with cirrhosis from a compensated to a decompensated state.
- It changes their prognosis as well as their quality of life.
- Early identification of patients at high risk of decompensation impacts surveillance and changes the treatment plan of the patients, likely improving their prognosis.
- At present, there is no simple, routinely performed serum marker-based score to predict phase transition in compensated patients with cirrhosis.
EPOD score formula:
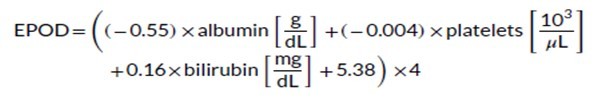
EPOD score consists of
- Platelet count in blood
- Albumin in plasma
- Total bilirubin concentration in plasma
Advantages of this score:
- High accuracy
- Non-invasive
- Estimated the probability of decompensation within the next 3 years
It utilises three different pathophysiological changes in early cirrhosis:
- Albumin - Reduction in hepatic synthesis
- Bilirubin - Impaired detoxification
- Platelets - Portal hypertension
- These are well-known surrogate markers of liver function and predictors of survival.
- These markers are also used as prognostic markers of survival in HCC patients resulting in the ALBI (albumin and bilirubin) and PALBI (platelets, albumin and bilirubin) scores.
Problems with already available CTP and MELD score
- These two scores were also tested as decompensation predictors but were outperformed by the EPOD score.
- Albumin and bilirubin are also part of the Child-Pugh score while the bilirubin is used in the MELD score.
- These two scores are designed for predicting survival, especially in late-stage cirrhosis.
- Therefore, their performance in predicting phase transition towards decompensation was limited.
- INR - used in both MELD as well as in the Child-Pugh score, is a suboptimal predictor in participants with liver diseases especially in a compensated stage.
- In addition to inter-laboratory variability, INR values in participants with cirrhosis have been shown to be unreliable.
HVPG measurement
HPVG is a marker of portal hypertension, but the invasive procedure is rarely justified in patients with compensated cirrhosis due to the risk of procedural complications.
What other studies found?
- Other studies identified anaemia and markers of systemic inflammation like IL-6 or vitamin D levels as predictors of decompensation.
- No data on IL-6 or vitamin D were available so far.
- Anaemia is indirectly represented by erythrocyte count, haematocrit and haemoglobin concentration.
- All three parameters were found to be strongly negatively associated with the risk of decompensation in the univariable regression analysis.
- Regardless of the cause, low erythrocyte count can lead to reduced microvascular oxygen distribution, thereby contributing to secondary organ failure or decompensation.
- Nevertheless, the erythrocyte count did not add predictive accuracy to a model of albumin, platelets and bilirubin and was, consequently, not included in the EPOD score.
- The reason for this might be that anaemia can have various causes, for example, malabsorption, occult bleeding, chronic inflammation or malnutrition.
What future study requires?
The effects of alcohol abstinence or hepatitis therapy on the EPOD score should be explored in the future.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Jimmy Patel is a practising gastroenterologist in Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries