Managing Obesity: Understanding the Basics
M3 India Newsdesk Oct 28, 2024
Obesity is a major public health challenge worldwide. This article explores the latest evidence-based dietary strategies for sustainable weight loss, emphasising their practical application in clinical settings.
Introduction
The prevalence of obesity is continuing to rise at an alarming rate. It is associated with numerous health complications, including Type 2 diabetes, cardiovascular diseases, certain cancers, and reduced life expectancy. The complexity of obesity lies not only in its multifactorial aetiology, encompassing genetic, environmental, and behavioural factors but also in the challenges of achieving and maintaining weight loss. Given the high rates of relapse in obesity management, there is an urgent need for evidence-based nutritional approaches that provide sustainable results.
Understanding the pathophysiology of obesity
Obesity results from an imbalance between energy intake and expenditure, leading to excessive fat accumulation. However, the simple model of "calories in versus calories out" is insufficient to fully capture the complexity of obesity.
Genetic predispositions, hormonal imbalances (such as leptin and ghrelin dysregulation), and an obesogenic environment all play significant roles.
Additionally, insulin resistance, often a consequence of obesity, further complicates weight management by promoting fat storage. Therefore, understanding the underlying pathophysiology is crucial for developing targeted, effective dietary interventions.
Evidence-based nutritional approaches
1. Calorie deficit and energy balance
- The cornerstone of weight loss is achieving a calorie deficit, where energy expenditure exceeds intake. However, the quality of calories consumed is equally important.
- Diets that emphasise nutrient-rich foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats are more effective for sustainable weight loss than those focusing solely on calorie reduction.
- Studies have shown that diets rich in high-fibre, low-glycemic index foods can improve satiety and reduce overall calorie intake without compromising nutritional quality.
- For instance, a study published in the New England Journal of Medicine found that participants on a high-fiber, low-glycemic index diet lost more weight and had better maintenance of weight loss compared to those on a traditional low-fat diet.
2. Macronutrient composition
- Low-carbohydrate diets: Low-carbohydrate diets, including the ketogenic diet, have gained popularity due to their effectiveness in rapid weight loss and metabolic improvements. By significantly reducing carbohydrate intake and increasing fat consumption, these diets induce ketosis, a state where the body burns fat for fuel. Evidence suggests that low-carb diets can lead to greater weight loss and better glucose control compared to low-fat diets, particularly in the short term. However, adherence can be challenging, and the long-term health impacts are still under investigation.
- High-protein diets: Protein plays a critical role in weight management due to its effects on satiety, thermogenesis, and muscle preservation. High-protein diets increase the production of satiety hormones like peptide YY and reduce levels of the hunger hormone ghrelin, which can help reduce overall calorie intake. A meta-analysis in The American Journal of Clinical Nutrition reported that high-protein diets not only enhance weight loss but also improve body composition by preserving lean muscle mass during calorie restriction.
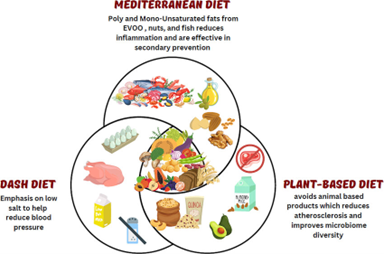
- Balanced diets (Mediterranean, DASH): Diets such as the Mediterranean and DASH (Dietary Approaches to Stop Hypertension) emphasise a balance of macronutrients, with an abundance of fruits, vegetables, whole grains, nuts, and healthy fats, particularly from olive oil and fatty fish. These diets are not only effective for weight loss but also offer additional cardiovascular and metabolic benefits. The PREDIMED study demonstrated that the Mediterranean diet, even when not calorie-restricted, led to significant reductions in body weight and waist circumference compared to a low-fat diet.
3. Intermittent fasting (IF)
Intermittent fasting (IF) involves cycling between periods of eating and fasting and includes approaches like the 16:8 method (16 hours fasting, 8 hours eating) and the 5:2 diet (five days of normal eating, two days of restricted intake). IF has been shown to improve metabolic flexibility, enhance fat burning, and reduce insulin levels. A study in Obesity Reviews found that intermittent fasting could be as effective as continuous calorie restriction for weight loss and may also improve metabolic health markers, including insulin sensitivity and lipid profiles.

4. Behavioural and psychological approaches
- Mindful eating: Mindful eating involves paying full attention to the eating experience, recognising hunger and satiety cues, and reducing emotional eating. Cognitive-behavioral therapy (CBT) techniques can help patients develop healthier eating habits and cope with triggers for overeating. A study in the Journal of Behavioral Medicine highlighted that mindful eating interventions led to significant reductions in binge eating episodes and improved weight loss outcomes in obese patients.
- Behavioural counselling: Incorporating behavioural counselling in dietary interventions can significantly improve adherence and long-term success. Techniques such as goal setting, self-monitoring, and positive reinforcement are crucial for helping patients make sustainable lifestyle changes.
Nutritional interventions in special populations
- Patients with comorbidities: Nutritional recommendations should be tailored for individuals with conditions like diabetes, hypertension, or polycystic ovary syndrome (PCOS). For example, low-carbohydrate, high-protein diets may be particularly beneficial for patients with insulin resistance, while the DASH diet is effective for those with hypertension.
- Cultural and socioeconomic considerations: Dietary advice must also consider cultural preferences and economic constraints. A culturally sensitive approach can improve patient engagement and adherence, leading to better outcomes.
Case study
Case study 1: Middle-aged male with metabolic syndrome
Patient profile
- Name: Mr. X
- Age: 45 years
- Diagnosis: Metabolic Syndrome
- BMI: 32 kg/m²
- Challenges: Elevated fasting glucose, high triglycerides, and hypertension.
- Intervention: Implemented a Mediterranean diet with a 20% calorie reduction, focusing on high-fibre vegetables, lean proteins, and healthy fats.
- Outcome: After 4 months, the patient achieved a 10% weight loss, improved insulin sensitivity, reduced triglycerides by 25%, and significant reductions in blood pressure.
- Lessons learned: This case highlights the effectiveness of a balanced, nutrient-rich diet that addresses both weight management and metabolic health.
Case study 2: Young female with PCOS
Patient profile
- Name: Ms. Y
- Age: 28 years
- Diagnosis: PCOS
- BMI: 30 kg/m²
- Challenges: Irregular menstrual cycles, and insulin resistance.
- Intervention: Low-carb, high-protein diet combined with intermittent fasting (16:8).
- Outcome: After 4 months, the patient experienced a 12% reduction in body weight, improved menstrual regularity, and enhanced insulin sensitivity.
- Lessons learned: This case demonstrates the benefits of macronutrient manipulation and eating pattern adjustments in managing obesity related to hormonal imbalances.
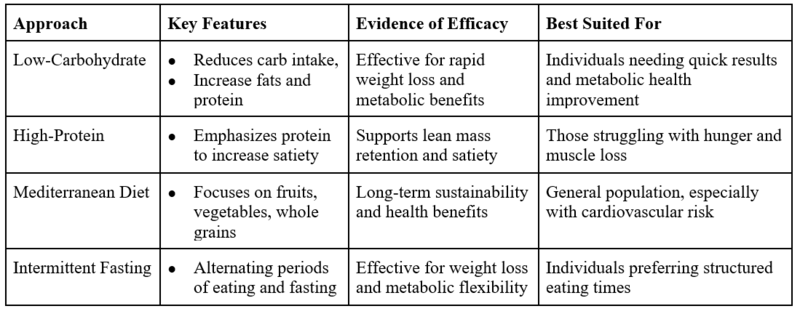 Table: Comparison of nutritional approaches for weight loss
Table: Comparison of nutritional approaches for weight loss
Conclusion
- Sustainable weight loss requires more than just reducing calorie intake; it involves adopting evidence-based nutritional strategies tailored to the individual’s physiological, psychological, and lifestyle needs.
- Clinicians should consider the quality of the diet, macronutrient composition, and the patient’s unique circumstances when recommending weight loss approaches.
- By employing a personalised, evidence-based approach, healthcare professionals can improve outcomes for patients struggling with obesity and its associated health risks.
- Future research should continue to refine these strategies and explore new interventions to enhance obesity management.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author of this article: Ms Rutambhara Nhawkar is a Clinical Dietician, M. Sc. (Clinical Nutrition & Dietetics), Certified Diabetes Educator and a medical writer from Pune.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries