Managing Cardiovascular Diseases through Diet Practices
M3 India Newsdesk Oct 22, 2024
This article provides an evidence-based approach to dietary and lifestyle changes that can significantly reduce the risk of CVDs, supported by clinical studies and two illustrative case studies.
Cardiovascular diseases (CVDs) remain the leading cause of death globally, accounting for approximately 17.9 million deaths annually. In India, CVDs are responsible for over 28% of all deaths, driven by urbanisation, dietary shifts, sedentary lifestyles, and increased prevalence of hypertension, diabetes, and dyslipidemia.
While pharmacological treatments have improved outcomes, diet and lifestyle modifications play a crucial role in both prevention and management.
Understanding cardiovascular diseases and modifiable risk factors
CVDs encompass disorders such as coronary artery disease, heart failure, hypertension, and stroke. Major risk factors include high blood pressure, dyslipidemia, diabetes, obesity, smoking, and physical inactivity. Addressing these modifiable risk factors can significantly alter the disease trajectory and reduce morbidity and mortality associated with CVDs.
1. Dietary modifications for cardiovascular risk reduction
Dietary modifications for cardiovascular risk reduction focus on adopting heart-healthy eating patterns, which emphasise a high intake of fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting processed foods, sugars, and sodium. These dietary changes improve lipid profiles, reduce blood pressure, decrease inflammation, and lower overall cardiovascular risk.

- Mediterranean diet: a proven heart-healthy diet
The Mediterranean diet emphasises whole foods, including fruits, vegetables, whole grains, legumes, nuts, and olive oil, with moderate fish and poultry intake and limited red meat and processed foods. This diet has shown significant benefits in reducing cardiovascular risk factors.
Key components and their impact:
- Monounsaturated Fats (Olive Oil): Reduces LDL cholesterol and improves HDL cholesterol levels.
- Omega-3 Fatty Acids (Fish): Lowers triglycerides, reduces inflammation, and improves endothelial function.
- Antioxidants (Fruits and Vegetables): Protects against oxidative stress and inflammation.
- Fiber (Whole Grains and Legumes): Lowers cholesterol and improves glycemic control.
Clinical evidence: The PREDIMED trial (Estruch et al., 2013) demonstrated that adherence to the Mediterranean diet, supplemented with extra-virgin olive oil or nuts, significantly reduced the incidence of major cardiovascular events by 30% compared to a low-fat diet.

- DASH Diet: Effective in hypertension management
The DASH diet, designed to combat hypertension, emphasises a high intake of fruits, vegetables, whole grains, lean proteins, and low-fat dairy while reducing sodium. It is particularly effective in lowering blood pressure, a major risk factor for CVDs.
Key components and their impact:
- High Potassium (Fruits and Vegetables): Helps reduce blood pressure.
- Low Sodium Intake: Decreases blood pressure and reduces stroke risk.
- Rich in Magnesium and Calcium: Enhances vascular health and supports blood pressure control.
Clinical evidence: Research has shown that the DASH diet lowers systolic and diastolic blood pressure by 11 and 6 mm Hg, respectively, in hypertensive patients, with additional benefits on lipid profiles and cardiovascular outcomes (Sacks et al., 2001).
- Plant-based diets: reducing cardiovascular risk
Plant-based diets, which emphasise whole plant foods and limit animal products, have shown promising results in reducing cardiovascular risk due to their high fibre, antioxidant, and phytochemical content.
Clinical evidence: A meta-analysis found that plant-based diets were associated with a 16% reduction in CVD risk and a 31% reduction in mortality from ischemic heart disease (Satija et al., 2017). Reducing red and processed meat intake has been linked to lower LDL cholesterol, blood pressure, and inflammation markers.
2. Lifestyle modifications for cardiovascular health
-
Physical activity: A pillar of cardiovascular fitness
Regular physical activity improves cardiovascular function, reduces blood pressure, enhances lipid profiles, and improves insulin sensitivity.
Recommendations:
At least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week.
Include muscle-strengthening activities at least twice a week.
Clinical evidence: Regular exercise is associated with a 20-30% reduction in coronary heart disease risk and significant improvements in blood pressure and HDL cholesterol levels (Naci & Ioannidis, 2013).
- Weight management: Critical for reducing cardiovascular risk
Obesity contributes to increased cardiovascular risk through hypertension, dyslipidemia, and insulin resistance. Weight loss improves blood pressure, cholesterol levels, and inflammatory markers.
Recommendation: A gradual weight loss of 0.5-1 kg per week through dietary modifications and physical activity is recommended.
Clinical evidence: A 5-10% reduction in body weight can lead to significant improvements in cardiovascular risk factors, especially in individuals with metabolic syndrome (Ryan & Yockey, 2017).
- Smoking cessation: reducing cardiovascular threats
Smoking is a major modifiable risk factor for CVDs, as it accelerates atherosclerosis, increases blood pressure, and promotes thrombosis.
Recommendation: Counseling, pharmacotherapy, and support groups are effective in smoking cessation.
Clinical evidence: Smoking cessation reduces the risk of coronary heart disease by 50% within the first year (Critchley & Capewell, 2003).
- Stress management: mitigating the impact on cardiovascular health
Chronic stress contributes to hypertension, arrhythmias, and other cardiovascular events. Techniques such as mindfulness, meditation, and yoga can mitigate these effects.
Clinical evidence: Stress reduction techniques like mindfulness-based stress reduction (MBSR) have been shown to improve blood pressure and heart rate variability, reducing cardiovascular risk (Jayasinghe, 2004).
Case studies
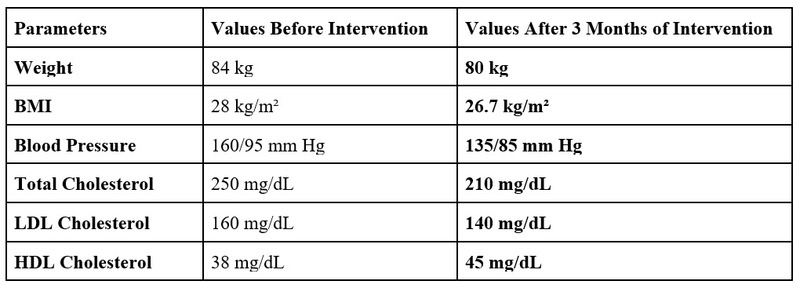
Case study 1: A 55-year-old male with hypertension and dyslipidemia
Background: Mr. A, a 55-year-old male with a history of hypertension and dyslipidemia, presented with elevated blood pressure (160/95 mm Hg) and total cholesterol of 250 mg/dL. He was overweight with a BMI of 28 kg/m². His lifestyle included a sedentary job, a high-sodium diet, and minimal physical activity.
Intervention: Mr. A was advised to adopt the DASH diet, reduce sodium intake to less than 2,300 mg/day, and increase potassium intake through fruits and vegetables. A physical activity regimen of 30 minutes of brisk walking five times a week was introduced.
Outcome: After 3 months, Mr. A reported increased energy levels with below changes in blood parameters and continued adherence to lifestyle changes.
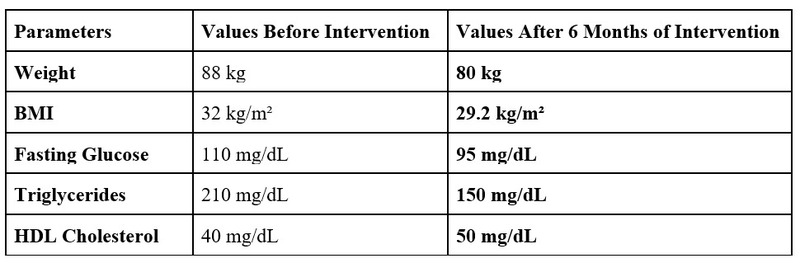
Case study 2: A 45-year-old female with obesity and pre-diabetes
Background: Ms B, a 45-year-old female with obesity (BMI 32 kg/m²) and pre-diabetes was referred for lifestyle intervention. Her lipid profile showed elevated triglycerides (210 mg/dL) and low HDL (40 mg/dL).
Intervention: A Mediterranean diet was recommended, focusing on increasing her intake of fruits, vegetables, whole grains, and healthy fats (olive oil, nuts). Ms. B was also encouraged to engage in moderate physical activity, such as yoga and cycling, for at least 150 minutes per week.
Outcome: After 6 months, Ms. B reported following blood parameters with better overall well-being.
Conclusion
Diet and lifestyle modifications are powerful tools in the prevention and management of cardiovascular diseases. By implementing evidence-based dietary patterns such as Mediterranean and DASH diets, promoting regular physical activity, supporting weight management, encouraging smoking cessation, and managing stress, healthcare professionals can effectively reduce cardiovascular risk. These interventions not only improve clinical outcomes but also empower patients to take control of their cardiovascular health.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author of this article: Ms Rutambhara Nhawkar is a Clinical Dietician, M. Sc. (Clinical Nutrition & Dietetics), Certified Diabetes Educator and a medical writer from Pune.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries