Latest ESH Updates on Hypertension (Part 2)
M3 India Newsdesk Sep 13, 2023
This article summarises the June 2023 guidelines from the European Society of Hypertension, offering doctors guidance on managing hypertension in patients with various health conditions, including comorbidities and pregnancy, for personalised care and treatment strategies.
Patients with hypertension frequently have coexisting diseases like diabetes, kidney disease, dyslipidemia, metabolic syndrome, cancer, and cardiovascular disease. The management of hypertension in patients with co-morbidity and in pregnancy is essential because such patients are more predisposed to target organ damage as compared to patients with isolated hypertension. This article deals with the management of hypertension in patients with co-morbidity as per the European Society of Hypertension 2023.
Recommendation for geriatric patients
Older patients with hypertension need active management as it has been associated with increased morbidity and mortality. A treating physician has to be careful while treating such patients to avoid adverse effects associated with treatment. To avoid adverse effects the ESH guidelines have given relaxation in blood pressure control with increasing age.
- Patients 65 to 79 years old
As per recommendation office threshold for initiation of drug treatment is 140/90 mmHg. The primary goal of treatment is to lower BP to <140/80mmHg. However, lowering BP to below 130/80mmHg can be considered if treatment is well tolerated.
- Patients 65 to 79 years old with ISH
The primary goal of treatment is to lower SBP in the 140 to 150 mmHg range. However, a reduction of office SBP in the 130 to 139 mmHg range may be considered if well tolerated, albeit cautiously if DBP is already below 70 mmHg. In older patients with isolated systolic hypertension, a combination of CCB and Thiazide/Thiazide-like diuretics can be used. However, all other major drug classes can be used.
- Patients ≥80 years old
As per the recommendation office, SBP threshold for initiation of drug treatment is 160 mmHg. However, a lower SBP threshold in the 140 to 160 mmHg range may be considered. Office BP should be lowered to an SBP in the 140 to 150 mmHg range and to a DBP < 80 mmHg. However, reduction of office SBP between 130 to 139 mmHg may be considered if well tolerated, albeit cautiously if DBP is already below 70 mmHg.
Additional recommendations
- Aggressive treatment is not advised in frail patients and does not aim to target office SBP below 120 mmHg or DBP below target for office SBP and DBP should be individualised.
- Reduction of treatment can be considered in patients age 80 years or older with a low SBP (<120mmHg or in the presence of severe orthostatic hypotension or a high frailty level
- Withdrawal of BP-lowering drug treatment on the basis of age, even when patients attain an age of ≥ 80 years, is not recommended if treatment is well tolerated.
- In older patients, treatment should start with lower doses and up-titration should be slower.
- The search for orthostatic hypotension in old patients should be systematic, even in the absence of symptoms. Back titration or discontinuation of BP-lowering drugs should be considered in patients with orthostatic hypotension.
Recommendations for LDL-cholesterol-lowering therapy in hypertension
Dyslipidemia has been associated with cardiovascular morbidity and mortality. Treating hypertensive patients with dyslipidemia should be prioritised by the treating physician as per guidelines.
- The decision to initiate LDL-cholesterol lowering treatment, as well as treatment goals, should be based on an estimation of total cardiovascular risk, with priority given to high-risk patients.
- As per recommendation statin remains the first choice of treatment in patients with hypertension and elevated CV risk. A maximum tolerated dose of statin should be prescribed to achieve LDL- cholesterol targets in patients with high CV risk.
- Ezetimibe may be added to the maximum tolerated statin dose to attain LDL-cholesterol targets.
- PCSK9 inhibitors and siRNA targeting PCSK9 may be considered in selected high-risk patients not attaining target LDL-cholesterol levels with statin/ezetimibe combination therapy.
- The use of a poly pill containing two BP-lowering drugs and a statin for LDL cholestrol lowering can be considered in hypertensive
Hypertension management in pregnancy
- In women with hypertensive disorders in pregnancy whether pre-existing or gestational hypertension, initiation or intensification of drug treatment is recommended when SBP is ≥ 140 mmHg and/or DBP ≥ 90 mmHg.
- In women with hypertensive disorders in pregnancy, too marked BP-lowering should be avoided. On-treatment DBP <80 mmHg is not recommended.
- Labetalol and α-methyl-DOPA are the first choice of BP-lowering agents for hypertensive disorders in pregnancy unless contraindicated.
- Extended-release nifedipine is recommended as an alternative BP-lowering agent during pregnancy. Up-titration of monotherapy should precede any combination drug treatment.
- Combination drug treatment between labetalol, extended-release nifedipine, or α-methyldopa may be reasonable to achieve the desirable BP target after the failure of up-titrated monotherapy.
- ACE inhibitors, ARBs, or direct renin inhibitors are not recommended during pregnancy.
- Aspirin (100-150 mg, at bedtime, weeks 11-35) should be administered in pregnant women at high or moderate risk of preeclampsia.
- Severe hypertension (≥160/110 mmHg) in a pregnant woman requires prompt hospital admission.
- In pre-eclampsia with severe features, magnesium sulfate should be administered without delay.
- HBPM can be a reasonable alternative to conventional office BP measurement to detect new-onset hypertension in women at risk for pre-eclampsia without pre-existing hypertension.
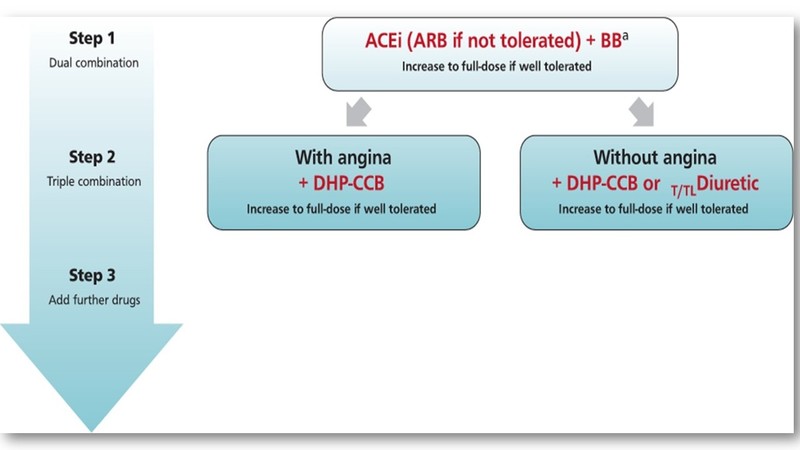
Treatment of hypertension in coronary artery disease (CAD)
- In adult patients with CAD, drug treatment should be initiated in the high-normal BP range (SBP ≥130 or DBP ≥80 mmHg).
- In patients with hypertension and CAD, it is recommended to use drugs with documented favourable effects in CAD such as ACEis (ARBs if not tolerated) or BBs.
- In patients with hypertension and CAD with angina pectoris, BBs and both DHP and non-DHP CCBs are particularly useful.
- Lowering heart rate to a range between 60 to 80 beats per minute is an additional treatment goal in hypertensive patients with CAD for which BB or non-DHP CCBs can be used.
- BBs should usually not be combined with non-DHP CCBs (e.g. diltiazem or verapamil).
- In patients with very low heart rate (< 50 beats per min) BB or non-DHP should be not initiated.
- Hypertension and LVH are frequently associated with myocardial ischaemia and no obstructive coronary artery disease (INOCA) including patients with myocardial infarction with no obstructive coronary artery disease (MINOCA). Treatment with RAS inhibitors, BBs, and CCBs can be used in this condition.
Treatment of hypertension in heart failure with reduced ejection fraction (HFrEF)
- In patients with hypertension and heart failure with reduced ejection fraction (HFrEF), it is recommended to combine drugs with documented outcome benefits including ACEis (ARBs if not tolerated), which could be substituted by ARNI (sacubitril/valsartan), BBs, MRAs, and SGLT2is, if not contraindicated and well tolerated.
- If patients remain with uncontrolled hypertension despite up-titration of drugs from the four major drug classes (RAS-inhibitors, BBs, MRAs, and SGLT2is) and use of additional treatment with a diuretic to manage fluid balance, a DHP-CCB can be added for BP control.
- The use of non-DHP-CCB is not recommended in HFrEF due to their pronounced negative-inotropic effect.
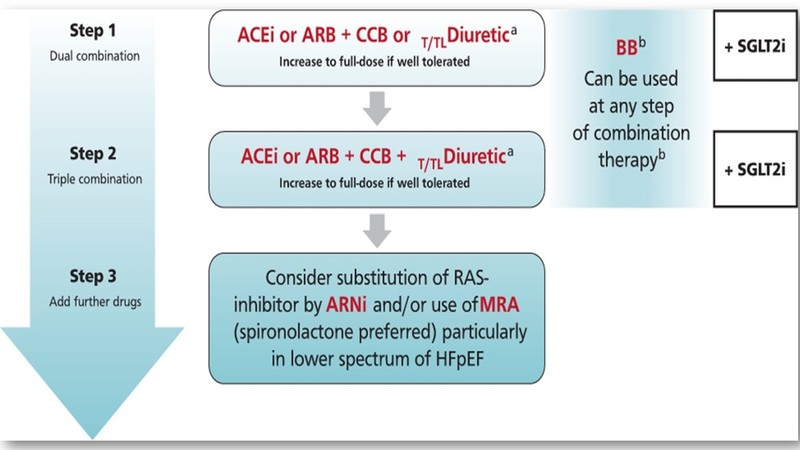
Treatment of hypertension in heart failure with preserved ejection fraction (HFpEF)
- Treatment of hypertension with all major antihypertensive drug classes (ACEis or ARBs, BBs, CCBs, and Thiazide/Thiazide-like diuretics) is recommended in patients with HFpEF.
- SGLT2is are recommended independently from the presence of type 2 diabetes.
- Substitution of a RAS-inhibitor by an ARNI (sacubitril/valsartan) can be considered, particularly in the lower HFpEF spectrum.
- Treatment with an MRA (spironolactone) regardless of diagnosed resistant hypertension can be considered, particularly in the lower HFpEF spectrum.
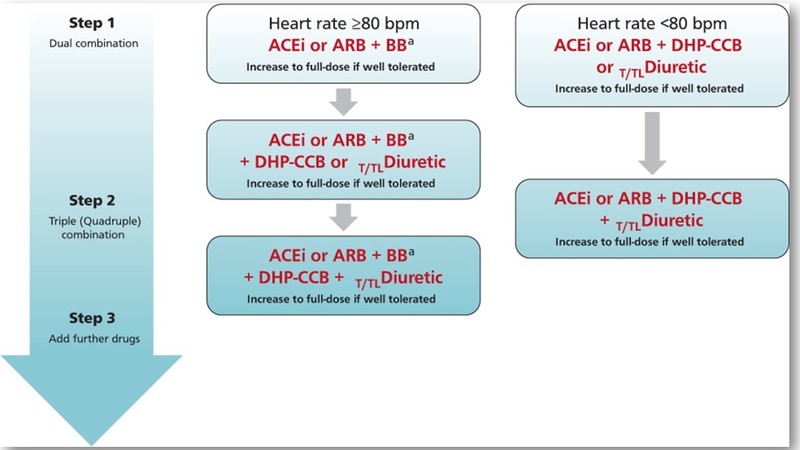
Treatment of hypertension in atrial fibrillation
- Treatment of hypertension reduces the risk of stroke and other CV outcomes in patients with AF. The BP threshold and targets as well as the drug treatment strategies should be the same as for the general hypertensive population.
- At least three office BP measurements by auscultation are recommended in patients with AF to account for the varying BP values.
- Automated oscillatory methods can be used for BP measurement in patients having AF because they satisfactorily measure SBP and only modestly overestimate DBP.
- BBs are the preferred drug class for heart rate control in patients having AF. Resting heart rate should be lowered below 110 beats per minute, targeting a heart rate < 80 beats per minute based on ECG analysis, particularly in symptomatic patients.
- Digoxin may be added to BBs to improve HR control in AF. BBs should usually not be combined with Non-DHP CCBs.
Management of patients with hypertension and AF during oral anticoagulation
- Stroke prevention with oral anticoagulants should be considered in AF patients with hypertension, even when hypertension is the single additional risk factor (CHA2DS2- VASc score of 1 in men and 2 in women).
- Initiation of oral anticoagulation should ideally start if SBP is below 160 mmHg. If SBP is ≥160 mmHg, it is recommended in priority to reduce BP to reduce the risk of major bleeding including intracranial haemorrhage.
- In hypertensive patients with AF receiving oral anticoagulation, the same treatment targets and choice of agents are recommended as for the general population.
- Non-DHP CCBs (Diltiazem and verapamil) for rate control should be used with caution because they may interfere with oral anticoagulants and increase bleeding risk.
Hypertension and cardiac valve disorders
- In patients with Aortic stenosis (AS), the BP thresholds and targets as well as the drug treatment strategies should be the same as for the general hypertensive population.
- In patients with high-grade AS, particularly with a history of syncope, BP lowering should be implemented more cautiously to avoid an excessive fall in BP and recurrent syncope.
- In patients with Aortic insufficiency, the BP thresholds and targets should be the same as for the general hypertensive population.
- Treatment with drugs reducing afterload, including RAS-blockers and CCBs, is recommended in patients with AI.
- Antihypertensive treatment is recommended to prevent MI and to reduce symptoms of MI, through reduced afterload of the left ventricle.
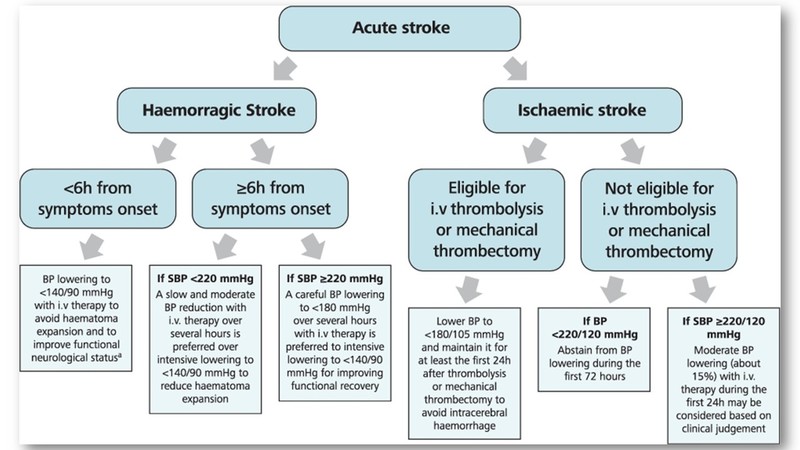
Management of blood pressure in acute stroke
- In patients with haemorrhagic stroke and < 6h after symptom onset, a BP <140/90 mmHg is recommended to avoid haematoma expansion.
- In patients with haemorrhagic stroke >6h after symptom onset, an SBP ≥220 mmHg may be carefully lowered with i.v. therapy to <180 mmHg. If SBP < 220 mmHg, slow and moderate BP reductions are preferable over intensive BP to <140/90 mmHg.
- In patients with acute ischemic stroke eligible for i.v. thrombolysis (IVT) or mechanical thrombectomy (MT), BP should be carefully lowered and maintained at <180/105 mmHg for at least the first 24 after intervention.
- In patients not eligible for IVT or MT with BP ≥220/120 mmHg, drug therapy may be considered based on clinical judgment, to reduce BP by 15% during the first 24 hours after the stroke onset.
Treatment strategies for diabetes
- Non-dipping or elevated night-time BP are frequent in type 2 diabetes and should be monitored by ABPM or HBPM.
- Antihypertensive treatment in type 2 diabetes is recommended to protect against macrovascular and microvascular complications.
- Immediate lifestyle interventions and antihypertensive drug treatment are recommended for people with type 2 diabetes when office SBP is ≥ 140 mmHg and DBP is ≥ 90 mmHg.
- Drug treatment strategies in patients with type 2 diabetes should be the same as for patients without diabetes but the primary aim is to lower BP below <130/80 mmHg
- BP control is difficult in diabetes and combination treatment is almost always necessary.
- SGLT2is are recommended to reduce cardiac and kidney events in type 2 diabetes. These agents have a BP-lowering effect.
- The non-steroidal MRA finerenone can be used, because of its nephroprotective and cardioprotective properties in patients with diabetic CKD and moderate to severe albuminuria. Finerenone has a BP-lowering effect.
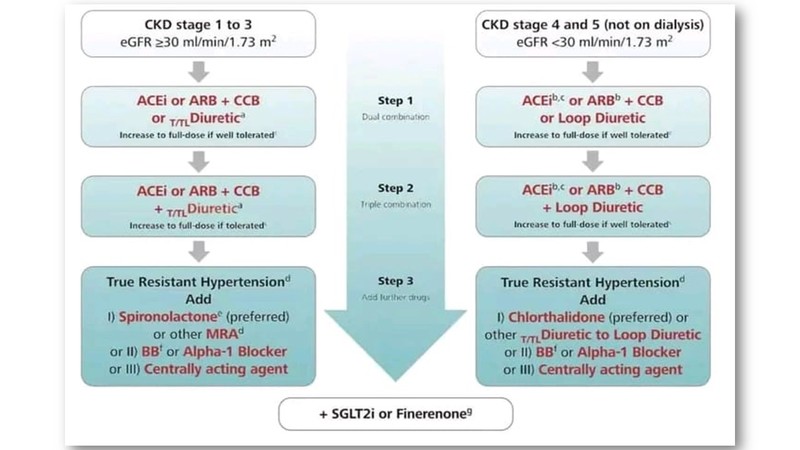
Treatment strategies in patients with kidney disease
- Non-dipping or elevated night-time BP are frequent in CKD patients and should be monitored by ABPM or HBPM.
- Immediate lifestyle interventions and antihypertensive drug treatment are recommended in most patients with CKD independently of the CKD stage if SBP≥ 140mmHg or DBP ≥90mmHg.
- In all patients with CKD, the primary goal is to lower office BP to <140 mmHg systolic and <90 mmHg diastolic.
- In most CKD patients (young patients, patients with an albumin/creatinine ratio ≥ 300 mg/g, high CV risk patients), kidney transplant patients with HTN office BP should be lowered to <130/80 mmHg if tolerated.
- In patients with CKD regardless of the presence of albuminuria, BP should not be lowered below 120/70 mmHg.
- An ACEi or an ARB, titrated to the maximum tolerated doses is recommended for patients with CKD and moderate (UACR 30 to 300 mg/g) or severe (UACR > 300 mg/g) albuminuria. A dual combination of an ACEi with an ARB is not recommended.
- SGLT-2 inhibitors are recommended for patients with diabetic and non-diabetic nephropathies CKD if eGFR is at least 20 or 25 ml/min/1.732.a
- The non-steroidal MRA finerenone is recommended in patients with CKD and albuminuria associated with type 2 diabetes mellitus if eGFR is at least 25 ml/min/1.732 and serum potassium <5.0 mmol/L.
- In CKD patients with hyperkalemia, a potassium binder can be used to maintain normal or near-normal serum potassium levels (<5.5 mmol/L) in order to allow optimal treatment with an RAS-blocker or an MRA to continue.
Hypertension management in obesity
- In adults with elevated BP who are overweight or obese, weight reduction is recommended to reduce BP and improve CV outcomes.
- Thiazide/Thiazide-like Diuretics and BBs have some unfavourable metabolic effects. However, since optimal BP control is the primary goal of antihypertensive treatment, combination therapy with these drug classes is frequently necessary and recommended.
- Dual GIP/GLP-1 RA or GLP-1 RA should not be prescribed for BP control in patients with obesity.
- Dual GIP/GLP-1 RA or GLP-1 RA or bariatric surgery lowers BP indirectly in parallel with body weight reduction and contributes to BP control in obese patients.
Hypertension treatment in glaucoma
- It is recommended that patients with hypertension >60 years old (or >40 years old in African Americans) be screened for glaucoma.
- In hypertensive patients with glaucoma, ABPM and closer ophthalmologic examinations should be associated with frequent BP measurements, including ABPM, particularly in patients with unexplained visual field deterioration.
- In patients with glaucoma, both very low and very high BP should be avoided, particularly during the night.
- In patients with glaucoma, bedtime administration of antihypertensive drugs should be avoided as it may increase the risk of excessive lowering of BP and thus visual field loss.
- BBs have been associated with lower intraocular pressure and decreased risk of primary open-angle glaucoma and may be preferred in hypertensive patients with glaucoma
Management of hypertension in cancer patients
- In patients with uncontrolled hypertension and BP values ≥180 mmHg for systolic and/or ≥110 mmHg for diastolic BP, it is not recommended to initiate anti-cancer therapy.
- Thiazide/Thiazide-like diuretics may be used only if needed for BP control and in patients with fluid retention, because of their potential to cause unwanted effects in cancer patients including increases in serum calcium concentration in patients with bone metastasis, increased risk of cardiac arrhythmias due to prolonging the QT interval by inducing hypokalaemia, increase the risk of hyponatremia, and potential worsening of hypovolaemic states or dehydration.
- Non-DHP CCBs should be avoided in cancer patients who are treated with anticancer drugs that are susceptible to pharmacokinetic interactions mediated by CYP3A4 and/or P-gp.
- Hypertension induced by VEGF inhibitors may be treated with either RAS inhibitors (ACEis or ARBs) or DHP-CCBs.
- In severely ill cancer patients, the treatment of hypertension should be individualised according to symptoms, co-morbidities and polypharmacy in a shared-decision making process.
Click here to read part 1- ESH 2023 Hypertension Guidelines
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist, physician and an obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries