Kounis syndrome: A primer
M3 India Newsdesk Dec 22, 2018
Dr. Manjula Sarkar, a senior Cardiothoracic Anaesthesiologist explains the diagnosis and treatment of allergic acute coronary syndrome, commonly known as Kounis syndrome.

Kounis syndrome also commonly known as allergic angina or allergic myocardial infarction is defined as the concurrence of acute coronary syndromes with conditions associated with mast cell activation, involving interrelated and interacting inflammatory cells, and including allergic reactions or hypersensitivity and anaphylactic or anaphylactoid attacks.
Although Kounis is not a rare condition, the diagnosis of it is often overlooked. The common causes include:
- numerous drugs- analgesics, anaesthetics, antibiotics, anticoagulants, antineoplastics
- environmental exposures
- pre-existing conditions such as asthma
- idiopathic anaphylaxis
- mastocytosis
Drug triggers for Kounis syndrome*
| Class | Chemical name |
| Analgesics |
Aspirin, Dipyrone |
| Anaesthetics |
Etomidate, Isoflurane, Midazolam, Propofol, Remifentanil, Rocuronium bromide, Succinylcholine, Suxamethonium, trimethaphan
|
| Antibiotics | Ampicillin, Ampicillin/Sulfactam, Amoxicillin, Amikacin, Cefazolin, Cefoxitin, Cerufoxime, Cephradine, Cinoxacin, Lincomycin, Penicillin, Sulbactam/Cefoperazone, Piperacillin/Tazobactam, Trimethoprim-Sulfamethoxazole, Sulperazon, Vancomycin |
| Anticoagulants | Heparin, Lepirudin |
| Anti-neoplastics | 5-fluorouracil, Capecitabine, Carboplatin, Denileukin, Interferons, Paclitaxel, Vinca Alkaloids |
| Contrast Media | Iohexone, Ioxaglate, Meglumine diatrizoate, Sodium indigotindisulfonate |
| Glucocorticoids | Betamethasone, Hydrocortisone |
| Nonsteroidal anti-inflammatory drugs | Alclofenac, Diclofenac, Naproxen |
| Proton pump inhibitors | Lansoprazole |
| Skin disinfectants | Chlorhexidine, Povidone-Iodine |
| Thrombolytics | Streptokinase, Tissue Plasminogen Activator, Urokinase |
| Others | Allopurinol, Bupropion, Clopidogrel, Dextran, Enalapril, Esmolol, Fructose, Gelofusin, Insulin, Iodine, Iron, Losartan, Protamine, Tetanus Antitoxin, Glaphenine, Mesalamine |
Other common triggers*
| Conditions | Food | Environmental Exposure |
| Angioedema | Actinidia Chinensis | Grass cutting |
| Anisakiasis | Canned fish (tuna) | Hymenoptera stings |
| Bronchial asthma | Fish | Jellyfish Sting |
| Churg-Strauss syndrome | Fruits | Latex contact |
| Exercise-induced anaphylaxis | Mushroom poisoning (Coprinopsis atramentaria) | Millet allergy |
| Food allergy | Shellfish | Scorpion Sting |
| Hay fever | Vegetables | Snake venom |
| Idiopathic Anaphylaxis | Tomato salad | Metals |
| Intracoronary stenting | ||
| Mastocytosis | ||
| Nicotine exposure | ||
| Scombroid syndrome | ||
| Serum sickness | ||
| Skin itching/scratching | ||
| Stents (bare metal, drug-eluting) |
The 3 variants of the syndrome
Type I variant:
- It includes patients with normal or nearly normal coronary arteries without predisposing factors for coronary artery disease, in whom acute allergic attacks can induce either coronary artery spasm alone without raised cardiac enzymes and troponins or coronary artery spasm leading to acute myocardial infarction with raised cardiac enzymes and troponins
Type II variant:
- It includes patients with culprit but quiescent pre-existing atheromatous disease in whom the acute allergic attacks can induce either coronary artery spasm, or plaque erosion or rupture manifesting as acute myocardial infarction
Type III variant:
- It occurs in the setting of coronary thrombosis (including stent thrombosis) where aspirated thrombus stained with hematoxylin-eosin and Giemsa demonstrate the presence of eosinophils and mast cells respectively
- It also includes people who have died suddenly after previous coronary stent insertion, where evidence of an allergic reaction to the stent is found on post-mortem examination
Pathophysiology of Kounis syndrome
- During hypersensitivity or during an allergic blow up, degranulation of mast cells takes place and a variety of stored and newly formed inflammatory mediators are released locally and within the systemic circulation, which include: biogenic amines such as histamine, chemokines, enzymes such as neutral proteases, chymase, tryptase, cathepsin-D, peptides, proteoglycans, cytokines, growth factors and arachidonic acid products such as leukotrienes, thromboxane, prostacyclin and platelet activating factor (PAF).
- Some of these mediators such as histamine, neutral proteases including tryptase, chymase and cathepsin-D, as well as arachidonic acid products such as leukotrienes, PAF and thromboxane have important cardiovascular actions.
- Histamine induces coronary vasoconstriction (the histamine test has been replaced nowadays by the ergonovine test), induces tissue factor expression and activity and activates platelets
- All three proteases, tryptase, chymase and cathepsin-D can activate matrix metalloproteinases, which can degrade the collagen cap and induce plaque erosion and rupture
- Tryptase exerts a dual action on the coagulation cascade with both thrombotic and fibrinolytic properties, but this action seems to depend on patient comorbidity and mast cell clonality
- Indeed, it was found recently that activating mutations exist in c-kit, that codes for KIT, the receptor for stem cell factor which is essential for mast cell development, proliferation, survival, adhesion and homing. This cascade of events results in a hyper-responsive mast cell phenotype with increased release of mast cells tryptase able to more easily induce Kounis syndrome and differentiate mast cell content actions.
- Chymase and cathepsin-D act as converting enzymes and convert angiotensin I to angiotensin II, which is a major vasoconstricting substance.
- Leukotrienes are also powerful vasoconstrictors and thromboxane and PAF are platelet activators with vasoconstricting properties.
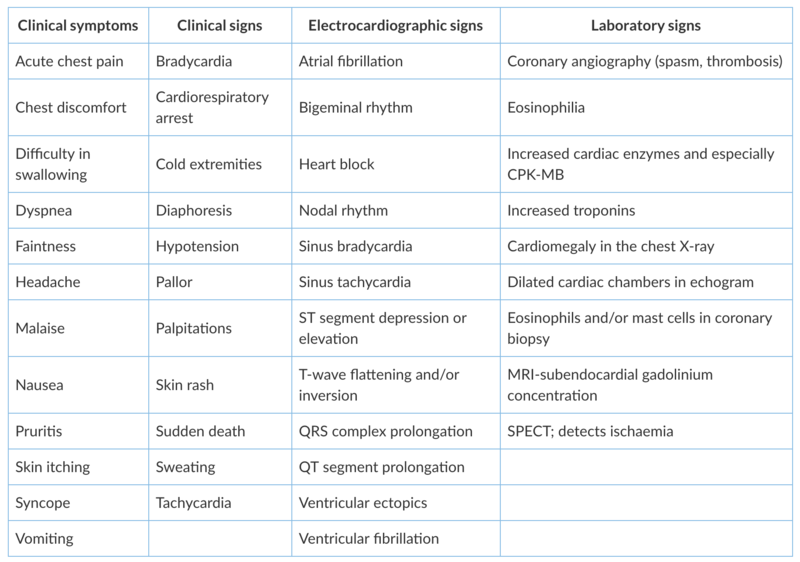
Signs and symptoms of Kounis syndrome
Allergic inflammation goes through three phases:
- the early phase which lasts minutes
- the late phase which lasts from 2 hours to 2 days
- the chronic phase which follows a continuous, persistent, and repetitive allergen exposure and lasts as long as the allergen is present
It seems likely that early (acute <24 hours and sub-acute 1 to 30 days), late (>30 days), and very late (>12 months) stent thrombosis correspond temporally with the early, late and chronic allergic inflammation independently of the level of documentation as definite or confirmed (symptoms suggestive of an acute coronary syndrome and angiographic or pathologic confirmation), probable (unexplained death within 30 days or target vessel myocardial infarction without angiographic confirmation), and possible (any unexplained death after 30 days).
Treatment protocol to be followed
Treatment of Kounis syndrome may be challenging because firstly, one needs to consider both cardiac and allergic symptoms simultaneously and secondly, the drugs administered for these manifestations can worsen allergy and aggravate heart function.
Type I variant
- Treatment of the allergic event alone can treat type I variant
- The use of intravenous corticosteroids such as hydrocortisone at a dose of 1 to 2 mg/kg/day and H1 and H2 antihistamines such as diphenhydramine at a dose of 1 to 2 mg/kg and ranitidine at a dose of 1 mg/kg are appropriate
- In addition, vasodilators such as calcium-channel blockers and nitrates can abolish hypersensitivity induced vasospasm
Type II variant
- An acute coronary event protocol together with corticosteroids and antihistamines should be applied
- Vasodilators such as nitrates and calcium blockers are given if needed
Type III variant
- The use of mast cell stabilizers in association with steroids and antihistamines should be recommended
- Harvesting of intrastent thrombus together with a histological examination of aspirated material and staining for eosinophils (hematoxylin and eosin) and mast cells (Giemsa) should be undertaken
- In patients who develop allergic symptoms following stent implantation, desensitisation measures should be applied
One should bear in mind that:
- Nitroglycerin causes hypotension and tachycardia, which may further complicate allergic reaction
- β-blockers can exaggerate coronary spasm due to unopposed action of α-adrenergic receptors
- Epinephrine is the drug of choice and can save lives in anaphylaxis, but in Kounis syndrome can aggravate ischemia and worsen coronary vasospasm
- In severe cases, sulfite-free epinephrine is preferable to be given intramuscularly because it has faster onset of action and more sustained levels as compared with the subcutaneous route (recommended intramuscular doses 0.2 to 0.5 mg [1:1000]) and an aqueous solution is preferable
- In patients with previous history of coronary heart disease who receive β-blockers epinephrine may be ineffective and may even induce more vasospasm due to unopposed α-adrenergic effect, therefore glucagon may be considered
- Opiates such as morphine, codeine and meperidine wich are usually given to relieve acute chest pain from myocardial infarction should be administered with extreme caution in patients with Kounis syndrome, since they can lead to massive mast cell degranulation and increase allergic reaction
- Fentanyl and its derivatives show slight mast cell activation and should be the drugs of choice when narcotic analgesia is necessary
*Reference: Kunis, N. (2016). MAST CELLS AND THE HEART: KOUNIS SYNDROME AND TAKOTSUBO CARDIOMYOPATHY. [online] TMS- The Mastocytosis Society. Available at: https://tmsforacure.org/expert-information/mast-cells-heart-kounis-syndrome-takotsubo-cardiomyopathy/ [Accessed 21 Dec. 2018].
The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries