Individual Donor Nucleic Acid Testing: A primer
M3 India Newsdesk Feb 08, 2018
Universal access to safe blood transfusion requires multi-sectoral approach and it does involve cost, however, unsafe blood transfusion is deemed costlier, both, in human and economic terms.

Attaining blood transfusion safety remains an uphill task due to a number of factors.Safe transfusion entails, not only the application of science and technology to blood processing and testing but it largely depends upon the social mobilization as well to voluntary blood donation by sufficient numbers of people who have no infectious disease.
A recent report released by National AIDS Control Organisation (NACO) revealed that between January 2015 to May 2016, 2,234 people in India were infected with HIV owing to blood transfusions.According to National Blood Policy (based on a Supreme court judgment that put the onus of providing safe blood on the government), every unit of blood that is donated at a blood bank should be thoroughly checked and tested to ensure that the blood does not contain any viruses or other pathogenic sources of infections.
Despite this, every other day there are cases of people being infected through blood transfusion. This is mainly due to the limitations of ELISA (Serology), a testing method, used in most blood banks, which poses challenges for detecting very early stages of infection in a donated unit of blood.
How big is this problem?
In India, there are almost 3,000 blood banks. Collectively, they process 90 lakh units of blood a year.
Various studies within our country (conducted by AIIMS New Delhi, Apollo Hospital Delhi, and many other prominent institutions) indicate that for every 1,000 units of blood donated, one unit would be deemed unsafe to transfuse.
Typically, every blood unit is transfused to two-three people in the form of separated components such RBC, Plasma, or platelets. This means every unsafe unit of blood can infect up to three persons.Going by these studies, we can estimate that almost 25,000 to 30,000 people get infected with HIV or Hepatitis B or C every year. This can be prevented.
How to prevent Transfusion Transmitted Infections or TTIs?
By adopting the advanced testing technique called ID-NAT, which offers the highest sensitivity and accuracy.
Many centres such as AIIMS New Delhi, RML New Delhi, CMC Vellore, and PGI Chandigarh are already performing ID-NAT tests. More blood banks must adopt this technology to ensure patient safety.
What is ID-NAT?
ID-NAT (individual Donor – Nucleic Acid Testing) is an international standard blood screening test where scientific evidence has shown that it has identified many cases of HIV and Hepatitis B & C infections that were not detected by conventional ELISA tests.
ID-NAT is more accurate and detects early stage infections also. By detecting earlier than conventional tests, it decreases the possibility of transmission of infection via transfusion.
How does the technology work?
Nucleic Acid Testing (NAT) is a molecular test for the detection of genetic material (RNA/DNA) of viruses such as HIV, Hepatitis B, and Hepatitis C that could be present in blood units received from donors. In NAT technology, even small amounts of viral genetic material, if present in a donor’s blood sample, is amplified by a billion-fold in the laboratory using special instruments. This results in early and specific detection of infected donors before the contaminated blood is transfused to a patient.
While every single donor sample has to be tested individually to obtain optimum accuracy, there are some blood banks that compromise testing methods by pooling/mixing multiple blood samples and perform one test on the sample mixture. Such mixing of multiple samples and performing one test on a mixture is called MiniPool NAT; and this is not the right way of doing NAT. This is mainly to cut cost, although at the expense of the patient’s safety.
The right way of performing NAT is Individual Donor NAT or ID-NAT, where each sample is tested individually.
How is it different from the existing solution?
The conventional technology known as Serology tests such as ELISA or Chemiluminescence Immunoassay (CLIA) depends on the infected person’s immune response to a particular infection such as HIV, HBV, or HCV. In ELISA/CLIA technology, antigens or antibodies produced by an infected person’s immune system gets detected as a surrogate marker for the viral infection and not the actual virus.
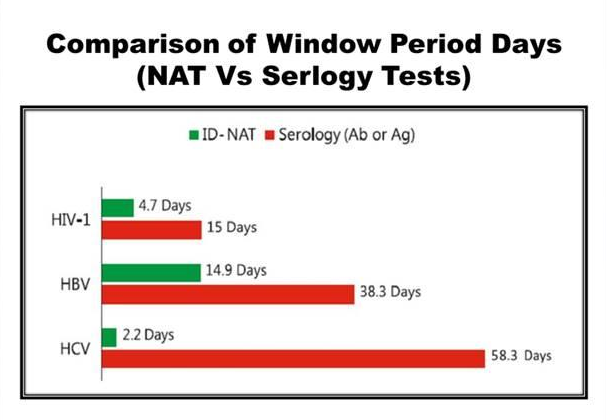
An infected person's body takes a sufficient amount of time t produce antigen or antibody during an infection. This time gap is called the window period of ELISA/CLIA test. If a blood donor donates blood after infection but within this window period, the current conventional technology (ELISA/CLIA) will not be able to detect that infection and will give a false negative result. These kind of otherwise infected but false negative resulted blood units are the biggest threat to our blood safety.
What are the benefits of using it in terms of cost, time, and effectiveness?
NAT directly detects viral RNA or DNA and can interdict an infection many days/weeks earlier than the conventional ELISA/CLIA tests. NAT also detects certain mutants, variants or hidden (occult) infections, which ELISA tests may miss. But remember, NAT is not a replacement technology for ELISA. It is an additional test for further safety. Current technology is mandatory as per the government of India and should be used irrespective of NAT implementation.
Who is using it?
This test, which is mandatory in many countries, continues to be optional in India. But there are a few hospitals and blood banks in India that have realised the importance of ID-NAT testing and have adopted this technique to screen blood.
Centres in India that have adopted this technique include AIIMS, New Delhi and Jodhpur, Gangaram Hospital, Indraprastha Apollo, and Fortis Hospitals in New Delhi, Medanta-The Medicity Gurgaon, PGI Chandigarh, Hinduja, HN and Ambani Hospitals in Mumbai, CMC Vellore, SIMS Chennai, and Amrita Institute, Kochi.. Recently, Stanley Medical College, Chennai has also commenced ID-NAT testing.
Karnataka government is the only state government in India that has made ID-NAT mandatory in all the government hospitals and blood banks.
There are more than 100 blood banks currently providing NAT-tested blood in India. But this number is too small since there are more than 2,700 licensed blood banks in the country. Less than 5% blood banks and less than 10% donated blood in India is currently NAT tested. Almost 90% of donated blood in India is not tested with NAT and carries the risk of causing TTI to patients due to a large window period of the current ELISA/CLIA tests. Most of the developed countries and many developing countries have made NAT mandatory decades ago.
Here is a what Dr. Aseem Tiwari, Director- Department of Transfusion Medicine, Medanta- The Medicity, Gurgaon has to say about the technology:
Dr. Tiwari has been using the technology for the last seven years. He said this is the best practice anybody can adopt. He said it is only a matter of time before everybody starts using this. "The only barrier is the price. But if I or my family is in need of blood, I would only go for NAT-tested blood. It is the standard test done in many countries.
Unfortunately, only a few hospitals in India practice this. It is as safe as scientifically proven in today's time. As of now, this is the safest blood test in the world. I would absolutely recommend this to my patients and family. It is the right of the patient to have access to the best equipment. Sadly, not many hospitals consider this," he said.
Information contributed by Mr. Sumit Bagaria, Indian Foundation for Safe Blood.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries