Impacted Wisdom Teeth and Its Treatment
M3 India Newsdesk Jul 10, 2024
This article explains what is an impacted tooth, its classification and aetiology. It also describes the various signs and symptoms associated with an impacted tooth along with its management.
Impacted tooth
An impacted tooth is a tooth which is completely or partially unerupted and is positioned against another tooth, bone or soft tissue so that its further eruption is unlikely, described according to its anatomic position.
Fully impacted wisdom teeth, partially impacted wisdom teeth and non-impacted wisdom teeth: What’s the difference?
Fully impacted wisdom teeth aren’t visible. They’re completely hidden underneath your gums.
A partially impacted wisdom tooth is slightly visible because part of it has erupted.
Non-impacted wisdom teeth have erupted and are completely visible above your gum line. It’s important to note that non-impacted wisdom teeth can still cause problems.
Classification of impacted third molar
The periapical radiograph or the orthopantomogram is used to analyse the impacted tooth for its classification.
Angulation of the impacted tooth (George Winter classification).
- Vertical
- Mesioangular
- Horizontal
- Distoangular
- Buccoangular
- Linguoangular
- Inverted
- Unusual
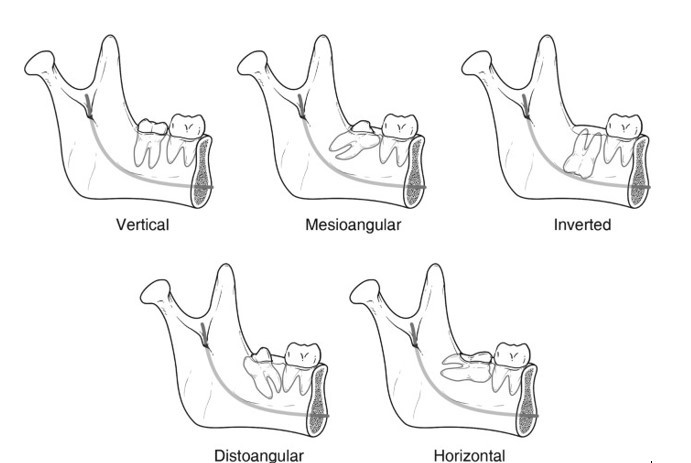
Angulation of the impacted tooth (George Winter classification)
Aetiology
Berger listed the following local causes for impaction of teeth:
- Irregularity in the position and pressure of an adjacent tooth.
- The increased density of the overlying or surrounding bone.
- Continued chronic inflammation with subsequent increase in density of the overlying mucous membrane.
- Lack of space due to underdeveloped jaws.
- Prolonged retention of the primary tooth.
- Early loss of primary tooth.
- Acquired diseases such as necrosis due to infection or abscess.
According to Berger, the following are the systemic causes of impaction:
- Prenatal causes: Hereditary and miscegenation.
- Postnatal causes: Rickets, anaemia, congenital syphilis, tuberculosis, endocrine dysfunction, and malnutrition.
- Rare conditions: Cleidocranial dysostosis, oxycephaly, progeria, achondroplasia, and cleft palate.
The following radiographs may be used for analysis:
- Intraoral periapical radiograph
- Occlusal X-ray of mandible
- Lateral oblique view of mandible
- Panoramic radiograph (Orthopantomogram)
Signs
- Pericoronitis and Pericoronal abscess: This is the most common cause for extraction of mandibular third molars (25–30%). Pericoronitis is frequently found to be associated with distoangular and vertical impaction. If treated inadequately, the infection may extend posteriorly resulting in submasseteric abscess.
- Dental caries: The incidence of caries of the second molar or third molar is about 15%.
- Periodontal diseases: Repeated food impaction and collection of food debris between the impacted third molar and the erupted second molar can lead to periodontal disease and subsequent bone loss. This weakens the bone support for the second molar and can cause pulpo-periodontal disease in the second molar.
Symptoms
- Radiating pain
- Swelling (intraoral or extraoral)
- Reduced and painful mouth opening
- Pus discharge
- Halitosis
Other indications of extraction
- Orthodontic reasons: Crowding of incisors, to facilitate orthodontic treatment, facilitate orthognathic surgery, and removal of third molars should be considered in the presurgical preparation for orthognathic surgery. Making bone cuts in Bilateral sagittal split osteotomies (BSSO) is easier after the third molars are removed.
- Odontogenic cysts and tumours.
- Resorption of the adjacent tooth root: Pressure from the impacted tooth can cause the root of the second molar to resorb.
- For placement of the dental prosthesis.
- Prevention of jaw fracture.
- Infection of deep fascial spaces: When pericoronitis is associated with an impacted tooth, infection can track into deep fascial spaces.
- To remove a potential infection source (e.g. before administration of radiotherapy)..
- Removal for autogenous transplantation.
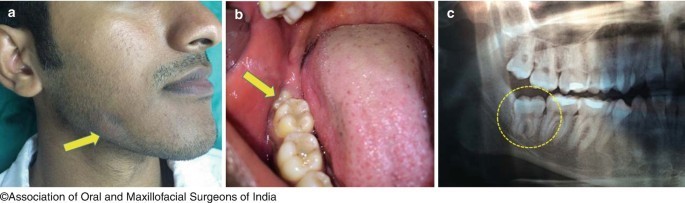
(a, b, c) Impacted right mandibular third molar with pericoronitis causing extraoral abscess (a) Extraoral abscess (Yellow arrow), (b) Impacted 48 with pericoronitis (yellow arrow), (c) OPG showing impacted 48 (Yellow circle)
Relative contraindications
- Compromised systemic status.
- Advanced age: Bone sclerosis increases with advancing age. This leads to poor healing, a larger defect size, and increased difficulty of the procedure. The risk of mandibular fracture is also high in these cases.
- Damage to any adjacent structures: If the inferior alveolar canal is in close contact with the impacted tooth, inadvertent damage can result in paresthesia.
- Questionable status of the second molar: If the second molar is badly decayed and unrestorable, removing it may allow the third molar to come into a functional position. The third molar may also serve as a bridge abutment. Such cases require multidisciplinary evaluation with the prosthodontist and endodontist.
- Deeply impacted third molars which do not appear to be associated with local or systemic pathology must not be removed.
Management techniques
Although the standard management strategy is usually considered to be surgical removal of the impacted tooth, the following methods listed below also should be considered depending upon the case:
- Conservative method: Leaving the tooth alone with regular follow-up clinically and radiographically. For instance, a deeply asymptomatic third molar may be left as such, especially in an older age group patient.
- Operculectomy: This procedure can be considered in a mandibular third molar that has partially erupted, and has sufficient space to come into occlusion, but is prevented from doing so by thick overlying mucoperiosteum. If the tooth still fails to erupt fully, it has to be considered for removal.
- Autogenous transplantation: Occasionally, the third molars can be considered for autogenous transplantation, usually to a first molar socket site. Because of the low success rate with such procedures, it is not widely used except in special circumstances.
- Orthodontically guided eruption: This is usually suited to impacted maxillary and mandibular canine teeth. Orthodontic guidance enables the tooth to reach a functional position within the arch. This technique can also be applied to impacted premolars and, in some instances, even impacted mandibular molars.
- Procedures that activate eruption: When indicated, these are usually applied to developing teeth.
Operative procedure
Any standard operative plan consists of the following stages:
- Placement of an incision to access the region of the impacted tooth.
- Removal of enough bone to allow for delivery.
- Sectioning the tooth and delivering it from the socket.
- Debridement of the surgical site.
- Wound closure.
- Followup
Supportive treatment
- Antibiotics
- Anti-inflammatory and analgesics
- Steroids
- Multivitamins
- Cold therapy immediately after the procedure
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Jalpa Patel is a practising dentist from Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries