Ibrutinib plus venetoclax: Dual therapy improves outcome in MCL
M3 Global Newsdesk Jul 25, 2018
New research in the New England Journal of Medicine states that treatment with ibrutinib plus venetoclax (ABT-199) improved outcomes over standard therapy in patients with mantle-cell lymphoma (MCL) and a poor prognosis.
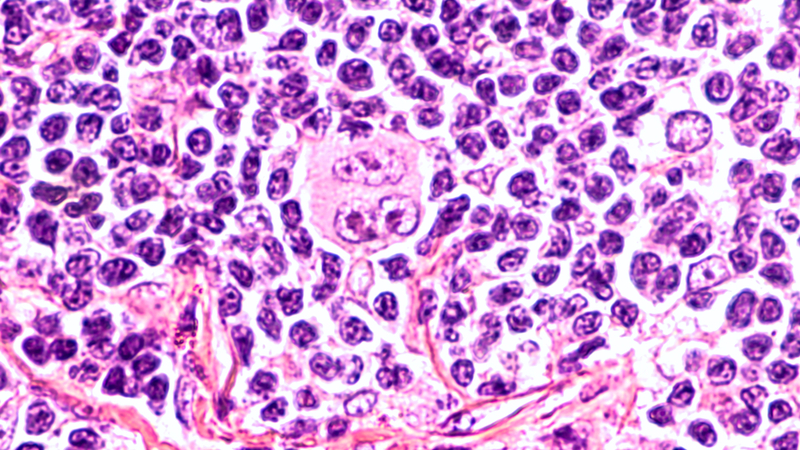
Currently, MCL is treated with targeted therapy for B-cell neoplasms, which includes ibrutinib, a BTK inhibitor, and venetoclax, an inhibitor of BCL2. Prior studies have reported that each has a complete response rate (CRR) of 21%. Preclinical models indicate that dual inhibition of BTK and BCL2 is synergistic. In addition, the agents have overlapping adverse events (AEs) that are generally minor.
The ABT-199 and Ibrutinib in Mantle-Cell Lymphoma (AIM) study, led by Constantine S. Tam, MD, from the Peter MacCallum Cancer Centre at the Royal Melbourne Hospital in Melbourne, Australia, was an open-label, single-group, phase 2 study that evaluated the combination therapy of ibrutinib plus venetoclax in patients with MCL.
Adult patients were eligible if they had relapsed or refractory MCL or if they were not candidates for cytotoxic chemotherapy.
To reduce the risk of tumor lysis syndrome (TLS), monotherapy with oral ibrutinib 560 mg daily was given for four weeks. Venetoclax 50 mg was added in week five, and the dose was increased in a step-wise, weekly manner to 400 mg orally each day—the recommended dose for treating chronic lymphocytic leukemia (CLL) at the time the study was conceived. Subsequently, based on an updated recommendation for MCL, the protocol was amended to allow escalation to venetoclax 800 mg daily after week 16 if complete response had not occurred.
Risk stratification for TLS was based on studies of venetoclax in patients with CLL, and it included tumor size and circulating lymphocyte count. The protocol was amended to include an additional ramp-up week of venetoclax 20 mg daily after TLS developed in two of 15 patients.
Disease reassessment was performed by CT scan, with and without 18F-fluoro-deoxyglucose–positron-emission tomography (PET). Minimal residual disease (MRD) was assessed by bone marrow exam and allele-specific oligonucleotide-polymerase chain reaction (ASO-PCR) at weeks four, 16, 28, 40, and 56.
Patients with known gastrointestinal involvement had gastroscopy and colonoscopy to confirm complete response. The Mantle Cell Lymphoma International Prognostic Index (MIPI)—which evaluates risk based on age, ECOG performance-status score, lactate dehydrogenase level, and white cell count—was calculated using published indexes.
Targeted amplicon sequencing of baseline tumor DNA and matched germline DNA was performed across 41 genes known to mutate in patients with lymphoma. The primary endpoint was rate of complete response at week 16, determined by tests other than PET.
A total of 24 consecutive eligible patients were enrolled: 23 had relapsed or refractory MCL with a median of two previous therapies, and one patient could not undergo cytotoxic chemotherapy. Most (88%) were male, and the median age was 68 years.
Half of the patients had aberrations of TP53, and 25% had an NF-κB pathway mutation; 75% had a high-risk prognosis based on the MIPI score.
Patients received study treatment for a median of 14.4 months; the median follow-up was 15.9 months. A total of six patients discontinued therapy due to disease progression, and two patients died without disease progression.
At week 16, the complete response rate according to CT without PET was 42%, which was higher than the historical result of 9% at that time point with ibrutinib monotherapy (P < 0.001). The rate of complete response as assessed by PET was 62% at week 16.
Overall, 71% patients had a PET-confirmed complete response as their best response. Among the 24 patients, absence of MRD was confirmed by flow cytometry in 16 patients (67%), and by ASO-PCR in 9 patients (38%).
Eight patients had disease progression, five were refractory to therapy, and three had a relapse after a complete response.
The most common AEs were generally low grade and included diarrhea (83%), fatigue (75%), and nausea or vomiting (71%). Serious AEs were noted in 14 patients, including TLS in two of the first 15 patients. No cases of TLS were reported after the protocol amendment to lower the starting dose of venetoclax.
No associations were apparent between response and age, number of previous therapies, previous autologous transplantation, ECOG performance-status score, bulky-node size, MIPI score, lactate dehydrogenase level, or IGHV mutational status.
Mutations were identified in all 24 patients using targeted sequencing of pre-study tumor specimens. Of the ten patients who presented with ATM mutations, all had a complete response. Responses were observed in patients with other gene mutations, but the investigators feel that larger studies of longer duration are needed to validate responses in genetically defined subgroups.
“Dual targeting of BTK and BCL2 with ibrutinib and venetoclax was consistent with improved outcomes in patients with mantle-cell lymphoma who had been predicted to have poor outcomes with current therapy,” concluded the authors.
To read more about this study, click here.
This story is contributed by Robyn Boyle and is a part of our Global Content Initiative, where we feature selected stories from our Global network which we believe would be most useful and informative to our doctor members.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries