Hysterectomy: Indications, Techniques, and Outcomes
M3 India Newsdesk Sep 23, 2024
This article discusses hysterectomy, including surgical options and outcomes, with a focus on minimally invasive techniques and special considerations for conditions like endometriosis. Key updates and case reports are also included to guide clinical practice.
A hysterectomy is an operation in which the uterus is removed. Removal of the Fallopian tubes, ovaries, and/or cervix may also be necessary. It may be done abdominally or vaginally. A vaginal hysterectomy is usually done for some cases of uterine prolapse.
What’s new?
- Hysterectomy for benign indications should preferably be approached by either vaginal or laparoscopic routes.
- Same-day discharge protocols following minimally invasive hysterectomy are safe.
- Correction of anaemia (haemoglobin <120 g/L) is indicated to reduce morbidity and mortality in the perioperative period.
- Opportunistic salpingectomy can be considered at the time of hysterectomy.
Indications
Refractory to medical treatment.
- Fibroids
- Endometriosis
- Uterine prolapse
- Cancer of the uterus, cervix, or ovaries
- Vaginal bleeding, DUB 20%
- Uncontrollable PPH
- Grade 4 prolapse uterus
- Pelvic inflammatory disease
- Severe pelvic adhesions
- Bilateral ovarian pathology
- Adenomyosis
- Pelvic congestion syndrome
- Intractable, recurrent dysmenorrhea or metrorrhagia or AUB refractory to medical treatment
- Recurrent intrauterine polyps
- Uterine perforation
- Mentally retarded patient with no hygiene control
- Pregnancy-Placenta increta, percreta, or accreta, atonic uterus, uterine perforation, ruptured uterus
Routes for hysterectomy
1. Abdominal hysterectomy (AH)
- Total
- Subtotal
2. Vaginal hysterectomy (VH)
3. Laparoscopically-assisted vaginal (LAVH)
- Totally laparoscopic hysterectomy
4. Caesarean hysterectomy
5. Robotic
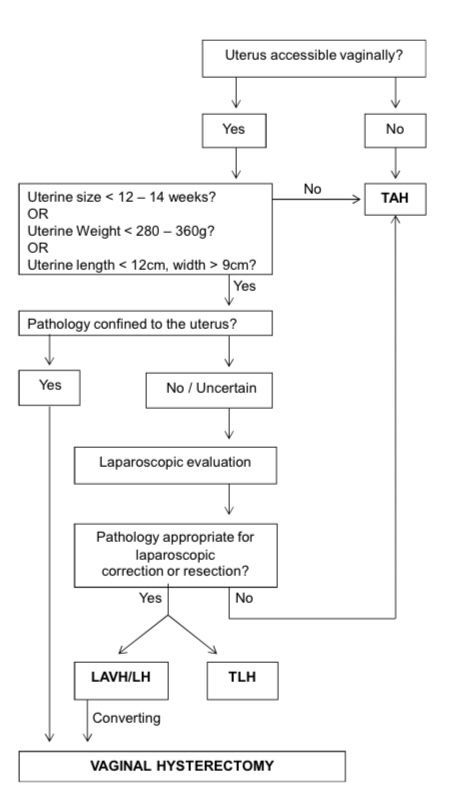
Which route is best?
1. Abdominal hysterectomy
- Results in greatest mean blood loss
- Has the highest incidence of febrile morbidity
- And abdominal wound infection (obviously)
- Longest hospitalisation
- And slowest to recover
2. Vaginal hysterectomy
- Is the preferred route when technically possible
3. Laparoscopic hysterectomy
- Requires training and equipment
- Longest operating time
- But the shortest hospitalisation and recovery
- But has the greatest overall risk of complications
- There is debate about its cost-effectiveness
4. Robotic hysterectomy
- 3-dimensional image
- Greater articulation
- Eliminate hand tremors
- Increased accuracy and precision
Conclusion
Vaginal hysterectomy is still considered the preferred route of hysterectomy, but laparoscopic hysterectomy is an appropriate alternative minimally invasive approach in suspected malignancy & severe endometriosis.
After hysterectomy
- Most women don't need Pap smears.
- Except those who had the previous CIN >2, Ca Cervix or Ca corpus uterus.
- Oestrogen-only HRT (ERT) is an option.
- Except when BSO was performed for oestrogen-responsive cancer or severe endometriosis.
- Symptom control in these patients can be a real problem.
- Current research suggests that ERT has many benefits and few risks.
Risks and side effects
- Earlier onset of menopause
- Greater risk of cardiovascular disease
- Increased chance of osteoporosis and bone fractures
- Uncontrolled urination
- Reduced libido
- Vaginal dryness
Summary statements
- Removal of normal ovaries at the time of hysterectomy decreases the risk of ovarian cancer but may be associated with health ramifications. Bilateral oophorectomy may lead to the acute development of menopausal symptoms in premenopausal women and has not been shown to offer a survival benefit in the absence of a genetic predisposition to ovarian cancer.
- Hysterectomy alone affects ovarian reserve.
- It is anticipated that opportunistic salpingectomy performed along with a hysterectomy will lower the risk of high-grade serous ovarian cancer.
- When a patient has a hysterectomy, routine uterosacral or vaginal vault suspension is not strongly supported by the available data.
What are the results of hysterectomy with ovarian preservation for endometriosis patients?
- Several retrospective studies have identified that hysterectomy may help with the long-term management of chronic pain associated with endometriosis. However, there is still a risk of recurrent pain post-hysterectomy when the ovaries are left in situ.
- Ovarian preservation at the time of hysterectomy is associated with an increased risk of recurrent pain and reoperation rates compared to hysterectomy plus BSO.
- Ovarian preservation is the recommended course of action for young women following a hysterectomy, as the dangers associated with surgical menopause must be weighed against the possible pain benefit of removing the normal ovaries. Nevertheless, the general risk of reoperation following a hysterectomy is low.
- Local excision of all extra-ovarian endometriosis should be emphasised in these circumstances.
What are the outcomes for patients with endometriosis treated with hysterectomy and concurrent BSO?
The implications of premenopausal oophorectomy are significant. Excision of all other endometriotic lesions is crucial for the best possible symptom control if definitive surgery, including a hysterectomy and BSO, is decided upon after thorough thought and patient discussion.
Numerous studies have demonstrated that if radical excision of all endometriotic lesions is combined with hysterectomy, whether with or without BSO, the long-term outcome (better quality of life, fewer reoperations) is favourable.
When endometriosis is present, there may be an increased risk of problems when using LH. Women with moderate to severe illness were almost four times more likely to experience surgical complications like
- Ureteral injury
- Bowel perforation
- Pelvic abscess
- Postoperative fever
- Avoiding dysfunction
Hormone therapy following surgery, whether systemic (oral or transdermal) or local (genitourinary syndrome of menopause) is useful in symptom management and morbidity reduction. There are data to support the importance of replacing hormones until the average age of menopause, which is 50 to 52.
Untreated symptoms, including
- Hot flashes
- Sleep problems
- Fatigue
- Decreased sexual desire
Anxiety, and depression, can have major ramifications on the quality of life and capacity to function.
Owing to the severe side effects of surgical menopause, it is advised that women retain their ovaries until they are at least 50 years old. The literature doesn't seem to have enough data to support strong pro- or con-recommendations for people over 60, yet one sizable study has found. For women who are not at genetic risk, there is no mortality advantage to BSO at any age.
It is advised that ovarian removal or retention should be discussed with each patient, highlighting her unique health risk factors, pelvic pathology, and personal preferences before undertaking a hysterectomy.
A. Case report- 1
-
A 44-year-old female patient presented to our gynaecology clinic with symptomatic uterine fibroids.
-
She had a known diagnosis of (ITP) for the past five years, which was managed with prednisolone therapy.
-
Biopsy results revealed normal bone marrow.
- Despite the treatment, her platelet count remained persistently low at 80000/μL.
- The patient had previously undergone a trial of medical management for her fibroids, including treatment with Mirenafollowed by Zoladex injection, but these interventions did not provide sufficient relief of her symptoms.
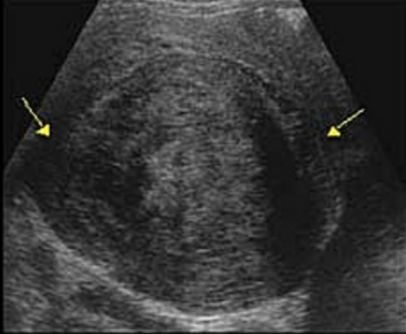
- Her initial ultrasound showed a large subserosa fibroid of 15/15/10cm on the dorsal aspect of the uterus.
Diagnosis
- Abdominal ultrasound showed a large subserosa fibroid on the dorsal aspect of the uterus.
- The patient experienced heavy and prolonged menstrual bleeding, which led to significant anaemia.
- The patient made an informed decision to proceed with (LAVH) following a comprehensive discussion of the possible risks and benefits of various treatment alternatives, including the limitations of medical management in her circumstances.
- The rationale behind the decision was to alleviate her symptoms, improve her quality of life, and address the underlying cause of her persistent anaemia.
- Preoperative assessment involves a collaborative effort between haematologists, anesthesiologists, and gynecologic surgeons. low platelet count of 80,000/μL and coagulation parameters were within normal range.
Treatment
- The patient's prednisolone therapy was optimised preoperatively, with the dose increased to 60 mg daily to suppress the immune response and improve platelet production.
- Platelet transfusion was planned two days before surgery to increase the platelet count to a safer range. The decision to perform a platelet transfusion was based on the patient's clinical symptoms, platelet count, and the anticipated surgical bleeding during LAVH.
- The transfusion aimed to raise the platelet count above 150,000/μL to minimise the risk of excessive bleeding intraoperatively.
- During LAVH, a meticulous surgical technique was employed, with an emphasis on hemostasis. Electrocautery was used cautiously, and precise suture ligation was performed to control bleeding from vascular structures.
- Intravenous tranexamic acid was used as a preventative step to lessen bleeding even further during the procedure. Throughout the procedure, the surgical team kept an eye out for any indications of bleeding or the formation of hematomas.
- Postoperatively, the patient was closely monitored in the intensive care unit for the first 24 hours. To keep a safe platelet level, platelet counts were monitored every day and additional transfusions were carried out as needed.
- The patient's postoperative course was uneventful.
B. Case report- 2
A 58-year-old woman G4P4A0came with the main complaint of a protruding mass coming out of her vagina for one year, which became worse with Valsalva. Difficulty in urinary or defecation was reported.,which Is relieved by manual insertion of the uterus inside the vagina.
Diagnosis
Physical examination revealed:
- A mass that protruded outside the hymen
- Uterine sondage was 10 cm
- The score for anal sphincter tone and levator ani muscle tone was 3.
- Negative results in cough test
- Prolapse reduction test
- Urinary residual test corresponding to stage 3 uterine prolapse
- Stage 2 cystocele
- Stage 2 rectocele
- Cervical elongation with cervical erosion
Transvaginal ultrasound revealed an anteflexed uterus size of 11 × 5 × 4cm with a cervical length of 6cm regular endometrium and endometrial thickness of 5mm, and no adnexal mass.
Treatment
- Total vaginal hysterectomy, bilateral salpingectomy, anterior colporrhaphy, colpoperineorrhaphy, and uterosacral ligament suspension were performed.
- On the second day following the procedure, the patient was released in good condition following an uneventful recuperation time.
- There were no indications of uterine pathology in the histology report. Three months later, at the follow-up, she had no problems.
Key messages
- Compared to laparotomy, minimally invasive hysterectomy (laparoscopic and vaginal) is linked to less complications.
- Hysterectomy for benign indications should preferably be approached by either vaginal or laparoscopic routes.
- Urinary tract injuries are comparable among surgical approaches to hysterectomy.
- Women with a normal risk of ovarian cancer should be advised of the harmful effects of bilateral oophorectomy on their health.
- Any more local endometriotic lesions should be completely removed in endometriosis patients having hysterectomy.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Sejal T Modi, MD, DGO practising in Mothers maternity and nursing home, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries