Handling bronchial asthma flare-ups during Diwali: Dr. Jyotsna Joshi
M3 India Newsdesk Nov 07, 2018
Dr. Jyotsna Joshi, a noted pulmonologist provides a comprehensive clinical management protocol for handling acute bronchial asthma flare-ups that are commonly reported as a result of air pollution caused during Diwali.
Use of fireworks during Diwali and the consequent detrimental effect on the air quality is widely recognised with elevated ambient air levels of particulate matter and its several metallic components and gases. Winter months see some of the worst air pollution levels. Diwali further leads to increased pollution.
Over a period of two days, Diwali adds about 40 μg/m3 to PM 2.5 particulate concentration. While this number may look small by itself, it is high considering the already poor air quality around the time. Acute flare-up of asthma is common during these periods. This review is intended to revisit asthma and its management including acute flare-ups during the festival season.
Asthma is a chronic, episodic disease of the airways. Asthma can be simply defined as reversible obstructive airway disease (ROAD) with bronchial hyper-reactivity (BHR).
- A survey done from Mumbai showed asthma prevalence of 3.5% by physician diagnosis, and 17% using a very broad definition including those with asymptomatic bronchial hyperreactivity
- The International Study of Asthma and Allergies in Childhood (ISAAC) has demonstrated a large variation in the prevalence of asthma (between 5 and 10%,) in children throughout the world including various regions in India
- The latest data on asthma outcome published by Centres for Disease Control (CDC) indicate that about 15 million American adults suffer from asthma
Acute flare-up of Bronchial Asthma
It is defined as an episode of worsening cough, dyspnoea and wheezing. The severity could range from mild to life-threatening and hence assessment of severity is necessary for treatment decision.
Fireworks and asthma flare-up
- Few investigators have identified the association between asthma and exposure to fireworks. According to researchers from the Institute of Environmental Assessment and Water Research (IDAEA-CSIC), metallic particles in the smoke emitted from the fireworks pose a health risk, particularly to asthmatics.
- In India, a 30% to 40% increase in the cases of wheezing, respiratory diseases, exacerbation of bronchial asthma, and bronchitis patients of all ages and gender were reported during the Divali festival. A published case report of one fatal and another near-fatal asthma exacerbation within hours of exposure to fireworks were identified.
Offering advice to asthmatics to avoid exposure as well as how to manage an exacerbation following exposure is crucial.
Diagnostic evaluation of asthma
- Diagnosis of asthma is considered in a patient who complains of dyspnoea with wheeze, chest tightness, and cough. These symptoms tend to be variable, initially intermittent and later persistent, particularly if untreated.
- History of other atopic condition i.e. allergic rhinitis, asthma, atopic dermatitis, eczema and urticaria in the family supports the diagnosis of asthma.
- Additional history of symptoms of gastro-oesophageal reflux disorder, exercise-induced worsening, nocturnal worsening, aspirin (or other drugs) hypersensitivity helps in assessing severity and making treatment decisions.
- History of medications for other medical conditions particularly systemic hypertension (B blockers or ACE inhibitors) must be elicited.
- Physical examination is usually unremarkable except the presence of rhonchi on auscultation.
Pulmonary function tests
Peak expiratory flow (PEF) is the fastest rate at which air can move through the airways during a forced expiration starting with fully inflated lung. Most adults and children, even as young as 5 years of age, can perform a PEF measurement. The effort required to produce measurement is a short maximal blast of air. The peak flow varies according to age, sex, and height. PEF monitoring is an important clinical tool at home in the office emergency department, and hospital.
PEF can be used for diagnosis if the:
- PEF increases more than 15%, 15 to 20 minutes after inhalation of rapid-acting β2-agonist (OR)
- PEF varies more than 20%
It is important to establish personal-best value.
Spirometry is useful in corroborating a diagnosis of asthma and in providing a longitudinal follow up of a given case. Spirometry in an asthmatic patient typically shows obstructive airway disease with reduced expiratory flow that improves with bronchodilator therapy i.e. reduced FEV1 / FVC ratio, reduced FEV1 and improvement in FEV1 after administration of inhaled bronchodilator by 12% and 200 ml. FEV1 % predicted is used to assess the severity of asthma.
Other investigations
- Chest radiograph: Hyperinflation is the most common finding on a chest radiograph. Chest radiograph is indicated when the diagnosis is in doubt or when there is a possibility of complications like pneumonia, pneumothorax, and allergic bronchopulmonary aspergillosis (ABPA).
- Laboratory tests: Haemogram often shows eosinophilia and total serum IgE may be elevated. Specific IgE against Aspergillus fumigatus is positive in ABPA.
- Skin allergen testing: Routine allergen testing in asthma is not indicated. It may be done to assess sensitivity to Aspergillus fumigatus if ABPA is suspected.
Treatment of acute severe asthma flare-up
Acute severe asthma (previously called Status Asthmaticus) is an attack of acute asthma not responding to routine therapy. Acute severe asthma requires hospitalisation and if it is life-threatening, intensive care management.
- Supplemental oxygen which should be initiated as soon as possible.
- Nebulised β2 agonist bronchodilators should be driven by oxygen.
- Outside the hospital, high dose β2-agonist bronchodilator may be delivered via large volume spacers or nebulisers.
- Nebulised ipratropium bromide (0.5 mg, 4-6 hourly) should be added to β2-agonist treatment for patients with acute severe or life-threatening asthma or those with a poor initial response to β2-agonist therapy.
- Oral corticosteroids in adequate doses (prednisolone 0.6 mg/kg) is given in all cases of acute severe asthma. Oral steroids are as effective as injected steroids, provided tablets can be swallowed and retained.
- Routine use of intravenous aminophylline is not likely to result in any additional bronchodilator compared to standard care with inhaled bronchodilator and oral steroids.
- Some individual patients with near-fatal asthma or life-threatening asthma with a poor response to initial therapy may gain additional benefit from aminophylline (5 mg/kg loading dose over 20 minutes unless on maintenance oral therapy) followed by an infusion of 0.5-0.7 mg/kg/h.
Non-invasive ventilation (NIV)
NIV is now well established in the management of ventilatory failure in acute exacerbations of COPD. Hypercapnic respiratory failure developing during the evolution of an acute asthmatic episode is regarded as an indication for urgent admission to intensive care.
It is unlikely that NIV would ever replace intubation in these very unstable patients but it has been suggested that this treatment can be used safely and effectively. Future studies might usefully examine its role in the gradually tiring patient, but at present, this treatment is not recommended.
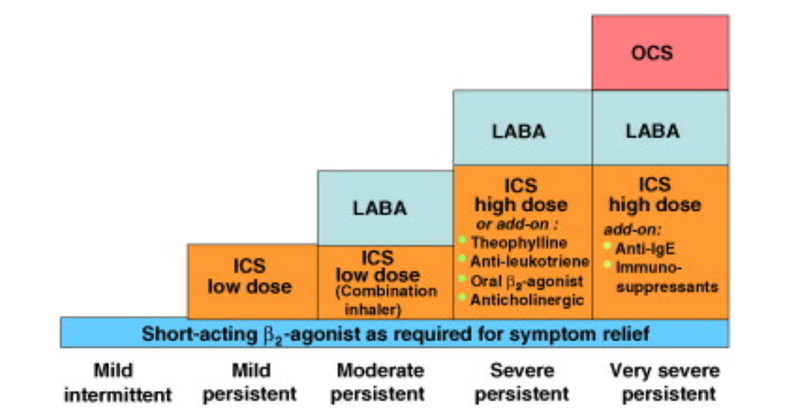
Step-care management of asthma
A stepwise approach aims to abolish symptoms as soon as possible and to optimise peak flow by starting treatment at the level most likely to achieve this. Patients should start treatment at the step most appropriate to the initial severity of their asthma. The approach allows early control, which is then maintained by stepping up treatment as necessary and stepping down when control is good (if control is sustained for at least 3 months).
The goal is to decrease treatment to the best medication necessary to maintain control. Review treatment every 3 to 6 months once asthma is under control.
Pharmacotherapy
The overall strategy is to use a stepwise approach based on level of severity.
- 'Reliever' or 'rescue' medications in the form of inhaled short-acting β2-agonist (SABA) are used on as needed basis are recommended for patients with very mild intermittent asthma who are asymptomatic between episodes
- Patients with persistent asthma (mild, moderate, or severe) are in addition treated with anti-inflammatory agents or 'preventer' medication primarily inhaled corticosteroids
- Patients with persistent asthma, with more frequent symptoms, are treated with the addition of anti-inflammatory agents, inhaled corticosteroids (ICS), 'preventer' medication used on a scheduled basis, along with reliever or rescue medications, on an as-needed basis
Note: Regular use of ICS apart from the anti-inflammatory action can also prevent asthma exacerbation, increase in bronchial hyperresponsiveness and accelerated loss of lung function. It also reduces mortality due to asthma.
- Additional, 'controller medications' like long-acting β2-agonists (LABA, theophyllines, anticholinergics (ipatropium, tiotropium) and anti-leukotrienes like montelukast are prescribed if asthma remains uncontrolled with ICS and SABA
These agents are also a rational alternative, taken in combination with inhaled steroids, in patients who remain symptomatic on low-intermediate inhaled steroid treatment. The benefits of combination therapy, as measured by symptom scores, as required use of beta-agonists, lung function, and exacerbation rates, with these other agents are not as dramatic, however, as with the addition of the long-acting inhaled bronchodilator.
Classification of asthma by severity
Global Initiative for Asthma (GINA) guidelines has classified bronchial asthma as intermittent mild persistent, moderate persistent or severe persistent depending on the severity of symptoms, peak expiratory flow rate, and FEV1.
Classification of asthma (modified from GINA guidelines)
| Steps | Symptoms/day | Symptoms/night | FEV1 |
| Step 1: Intermittent | Monthly symptoms | No | ≥80%, no PEF variability |
| Step 2: Mild persistent | Weekly symptoms | Monthly episode | ≥80%, no PEF variability |
| Step 3: Moderate persistent | Daily attacks symptoms | Weekly episode | 60 to 80% |
| Step 4: Severe persistent | Continuous symptoms | Frequent episode | ≤60% |
Pathogenesis of asthma
- Asthma is a heterogeneous disease, and this has been established by a variety of studies, which have indicated disease risk from susceptible genes, early environmental factors, and subsequent disease conduction.
- It has been long known that the tendency to develop allergy is inherited. Atopy has defined asthma as a genetic predisposition for the development of IgE-mediated hypersensitivity to allergens.
- Atopy can be recognised as a family history of allergic rhinitis, bronchial asthma, eczema, atopic dermatitis, and urticaria. Atopy, an autosomal dominant inherited trait is the most important risk factor, increasing the risk for the development of asthma by 10- to 20-fold.
- Ninety percent of atopic asthmatics have at least one atopic parent. Environmental factors lead to the selection of the asthma phenotype. Following inhalation of an allergen in an atopic subject inhaled allergens (inducers) are presented to the lymphocytes. The Th2 lymphocytes start a cascade of immune reactions.
- On subsequent exposure, the antigen directly interacts with the IgE antibody on the mast cells and release mediators, which cause bronchospasm. The hallmark of asthma is airway hyperresponsiveness and airway inflammation that result in chronic nonreversible changes due to airway remodeling.
Criteria for patient discharge
Although the diurnal variability of PEF is not always present during an exacerbation, evidence suggests that patients discharged with PEF<75% best or predicted and with diurnal variability >25% are at greater risk of early relapse and readmission. Patient should be on discharge medications 24 hours before discharge.
Prevention tips to give to patients
Sensitisation to inhalant allergens, including dust mite/mold spores/cat /dog /other animal proteins, cockroach and other insects, as well as outdoor pollen, is common among asthmatic patients. Routine measures of dust control and avoidance of obvious triggers is important. An elaborate search for the offending allergens and avoidance is cumbersome and not necessary. Simple measures to avoid exposure to these allergens are shown below.
Common asthma risk factors and action to reduce exposure
| Risk Factor | Action |
| Domestic dust mite allergen |
|
| Allergen from animals with fur |
|
| Cockroach allergy |
|
| Outdoor pollen, mold, and pollution |
|
However, patients with asthma at any level of severity should avoid:
- Exposure to environmental tobacco smoke
- Exposure to air pollution
- Use of beta-blockers
- Sulfite-containing containing food and beverages
- Pneumococcal and yearly influenza vaccines are also recommended
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries