Genetic variants linked to increased heart attack risk despite statin therapy
M3 Global Newsdesk Jun 29, 2018
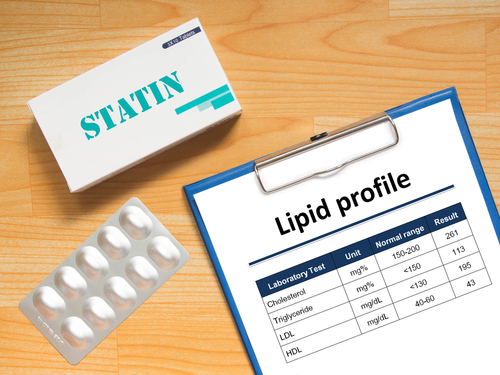
Seven genetic variants on the LPA gene were associated with an increased risk for heart attack and coronary heart disease (CHD) regardless of the cholesterol-lowering effects of statin therapy, according to results of a new genome-wide association study published in Circulation.
“People with these genetic variants were at a higher risk for heart disease, even considering those who have ideal cholesterol levels on their statin,” said corresponding author Joshua Denny, MD, MS, professor, Biomedical Informatics & Medicine, and director, Center for Precision Medicine, Vanderbilt University Medical Center, Nashville, TN.
The results of the study suggest that drugs targeting the LPA variants could lower the risk for CHD events in patients on statins, the researchers noted.
Although statin therapy decreases the incidence of CHD events, these events still occur despite reduced levels of low-density lipoprotein (LDL) cholesterol. How genetic variation contributes to CHD risk during statin therapy remains unknown.
For this investigation, researchers conducted a multisite genome-wide association study to find the genetic determinants of CHD events (defined as heart attack or the need for coronary revascularization) that occur during statin therapy.
The team searched 4 sites in the Electronic Medical Records and Genomics (eMERGE) network, a consortium of US cohorts with DNA samples linked to electronic health record data for conducting large-scale genetic research. This search identified 3,099 patients who had CHD events while on statin therapy, as well as 7,681 controls who were also on statins but had no CHD events.
The meta-analysis found 7 single nucleotide polymorphisms (SNPs) within the LPA/PLG locus that were associated with CHD events in patients on statins.
One SNP on the LPA gene was associated with the greatest increased risk of CHD events in patients on statin therapy (odds ratio [OR]=1.71, 95% CI 1.14-2.57, P=0.009). The researchers found that the minor allele of this SNP was associated with a 58% increase of CHD risk in statin-treated patients. This SNP was also associated with increased odds of CHD events independent of statin-induced reductions in LDL cholesterol. The link occurred even in patients with LDL cholesterol levels of 70 mg/dL and below.
The causal role of LP (a)
This SNP is known to be associated with circulating Lp(a) levels. Lp(a) is a particle formed by apolipoprotein (a), which is encoded by the LPA gene. Lp(a) is also an independent predictor of CHD. The findings from this study suggest that Lp(a) plays a causal role in CHD risk for patients on statins, the researchers concluded.
“The study highlights the need to consider targeting Lp(a) levels as an important independent factor to reduce cardiovascular risk in patients on statin therapy,” said the paper’s first author, Wei-Qi Wei, MD, PhD, assistant professor, Biomedical Informatics, Vanderbilt University School of Medicine.
Existing or new drugs that lower Lp(a) levels could reduce CHD events in patients on statins who carry LPA genetic variants, Dr. Wei predicted.
This study was supported by eMERGE Network (Phase III), as well as the National Institutes of Health and the American Heart Association.
This story is contributed by John Murphy and is a part of our Global Content Initiative, where we feature selected stories from our Global network which we believe would be most useful and informative to our doctor members.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries