Gastrointestinal Bleeding: Evaluation, Management and Referral Criteria
M3 India Newsdesk Jul 13, 2024
This article provides a comprehensive overview of gastrointestinal (GI) bleeding, including its types, clinical presentation, evaluation methods, management strategies, and criteria for referral.
Gastrointestinal (GI) bleeding is a potentially serious medical condition that requires prompt evaluation, appropriate management, and sometimes referral to specialised care. It can manifest in various forms and severity levels, necessitating a structured approach to both acute intervention and long-term care.
An overview of gastrointestinal bleeding
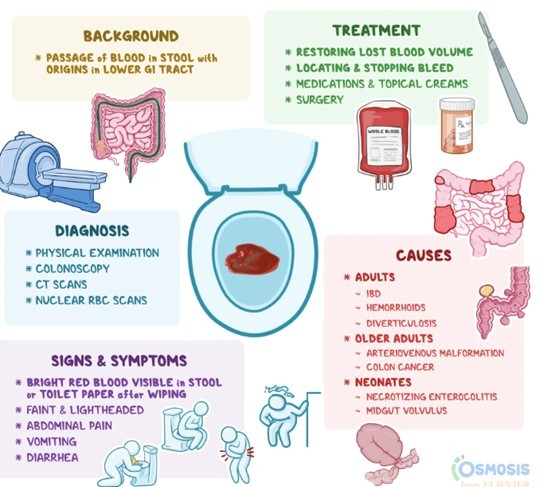
Gastrointestinal bleeding refers to any bleeding that occurs within the digestive tract, from the mouth to the rectum.
It can be classified into:
- Upper GI bleeding (UGIB), which originates proximal to the ligament of Treitz- UGIB commonly involves the oesophagus, stomach, or duodenum.
- Lower GI bleeding (LGIB), occurs distal to this point- LGIB typically involves the colon or rectum.
Types of gastrointestinal bleeding
1. Upper GI Bleeding (UGIB)
- Peptic ulcer disease: Gastric and duodenal ulcers can erode blood vessels, leading to significant bleeding.
- Esophagitis: Inflammation of the oesophagus, often due to gastroesophageal reflux disease (GERD), can cause erosions and bleeding.
- Varices: Enlarged veins in the oesophagus or stomach, commonly due to portal hypertension in liver cirrhosis, are prone to rupture.
- Mallory-Weiss Tears: Longitudinal mucosal lacerations at the gastroesophageal junction, often associated with vomiting.
2. Lower GI Bleeding (LGIB)
- Diverticular Disease: Bleeding from the diverticula (small pouches) in the colon is a common cause of LGIB.
- Colitis: Inflammatory bowel diseases (e.g., Crohn's disease, ulcerative colitis) and infectious colitis can lead to bleeding.
- Angiodysplasia: Abnormal blood vessels in the colon are prone to bleeding, especially in older adults.
- Colorectal cancer: Tumors in the colon or rectum may bleed intermittently or continuously.
Clinical presentation
The presentation of GI bleeding can vary widely depending on the location and severity of the bleeding. Common symptoms include:
- Hematemesis: Vomiting of blood (bright red or coffee-ground appearance).
- Melena: Black, tarry stools indicate digested blood.
- Hematochezia: Passage of bright red blood through the rectum.
- Abdominal Pain: Often localised to the area of bleeding.
- Weakness, Dizziness, or Syncope: Symptoms of significant blood loss.
Initial evaluation and assessment
When a patient presents with suspected GI bleeding, a systematic approach is crucial:
- History and physical examination: Detailed history to identify risk factors (e.g., NSAID use, alcohol consumption) and thorough examination to assess hemodynamic stability.
- Laboratory tests: Including complete blood count (CBC), coagulation profile, and basic metabolic panel to evaluate for anaemia and electrolyte abnormalities.
- Endoscopy: Urgent esophagogastroduodenoscopy (EGD) for UGIB and colonoscopy for LGIB are often required to identify the source and potentially treat the bleeding lesion.
Diagnostic imaging
Imaging studies play a role in evaluating patients with GI bleeding, especially when endoscopy is inconclusive or unavailable:
- Tomography (CT) Angiography: Useful in identifying active bleeding or vascular abnormalities.
- Nuclear scintigraphy (tagged red blood cell scans): Helpful for detecting intermittent bleeding sources, especially in LGIB.
Risk stratification
Assessing the risk of adverse outcomes guides management decisions:
- Rockall score (for UGIB): Predicts mortality based on clinical and endoscopic findings.
- Glasgow-Blatchford score (for UGIB): Predicts the need for interventions such as blood transfusion or endoscopic therapy.
- Clinical risk stratification tools (for LGIB): Help determine the need for hospitalisation and urgent intervention based on clinical parameters.
Long-term management and follow-up
After stabilising acute bleeding episodes, ongoing management focuses on:
- Treating underlying causes: Such as peptic ulcer disease, diverticular disease, or inflammatory bowel disease.
- Preventing recurrence: Lifestyle modifications (e.g., smoking cessation, avoiding NSAIDs) and medications (e.g., proton pump inhibitors) may be necessary.
- Surveillance: Regular follow-up with endoscopy or colonoscopy to monitor healing and detect recurrence of bleeding or underlying pathology.
Referral criteria
Referral to a gastroenterologist or a specialised GI bleeding centre should be considered in the following situations:
- Severe bleeding: Persistent hemodynamic instability despite initial resuscitation efforts.
- Complicated bleeding: Inability to identify or manage the bleeding source adequately with available resources.
- High-risk lesions: Such as large varices or suspected malignant lesions requiring expert intervention.
Conclusion
The evaluation and management of gastrointestinal bleeding require a multidisciplinary approach involving emergency physicians, gastroenterologists, and sometimes surgeons. Timely intervention and appropriate risk stratification are essential for optimising outcomes and reducing morbidity associated with this potentially life-threatening condition. Through systematic assessment, effective treatment, and diligent follow-up, healthcare providers can ensure comprehensive care for patients with GI bleeding.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Akshayaa is a General Practitioner at Sri. Balaji Heart Centre, Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries