Empowering Physicians: A Nutritional Blueprint for Effective Weight Loss Management
M3 India Newsdesk Sep 16, 2024
Physicians often face challenges in managing patients' weight, crucial for preventing chronic diseases. This article offers a clear, evidence-based approach to weight loss, helping physicians integrate effective dietary strategies into their practice.
The foundation of weight loss: Energy balance
While physicians possess a strong foundation in the science of medicine, the nuances of diet and nutrition may not be within their immediate expertise. The cornerstone of weight loss is energy balance; the relationship between calories consumed and calories expended.
While this concept is universally recognised, the practical application of managing energy intake through diet is often misunderstood. It’s crucial to understand that not all calories are created equal. The macronutrient composition of a diet- proteins, fats, and carbohydrates; plays a significant role in satiety, metabolism, and overall weight management.
1. A balanced diet with macronutrient distribution
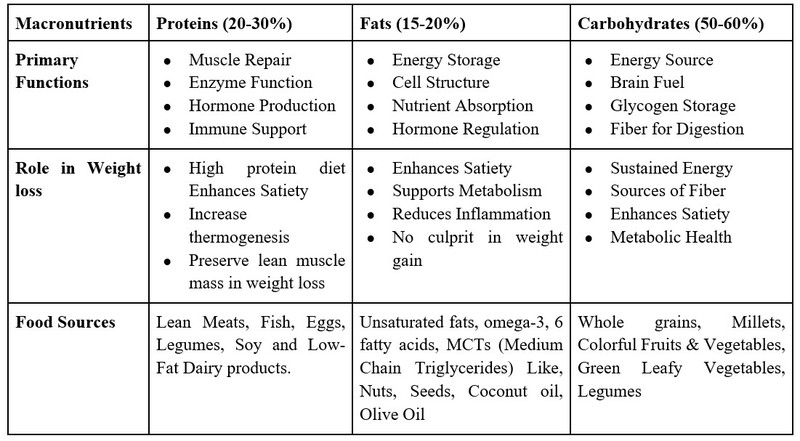 A Balanced Diet with Macronutrient Distribution
A Balanced Diet with Macronutrient Distribution
A guide to macronutrients
2. The role of fibre
Dietary fibre, particularly soluble fibre, is essential in weight management. It slows gastric emptying, increases satiety, and modulates the gut microbiota, which plays a role in metabolism. A daily intake of 25 to 30 grams of fiber, from sources such as vegetables, fruits, legumes, and whole grains, is recommended.
3. The importance of meal timing
Emerging evidence suggests that when patients eat may be just as important as what they eat. Circadian rhythms influence metabolic processes, and meal timing can affect weight loss outcomes. Physicians should guide patients towards eating within a consistent daily time window, ideally aligning with their natural circadian rhythm. Intermittent fasting, such as the 16:8 method (16 hours fasting, 8 hours eating), can be a useful strategy for some patients.
4. Behavioural strategies in weight management
Behavioural modification is crucial in sustaining weight loss. Physicians should encourage patients to adopt the following strategies:
- Mindful eating: Patients should be guided to eat slowly, recognising hunger and fullness cues, which can prevent overeating.
- Portion control: Educating patients on portion sizes can help manage caloric intake without the need for complex calorie counting.
- Regular monitoring: Encourage patients to track their food intake, physical activity, and weight regularly. This not only aids in accountability but also allows for early intervention if weight gain occurs.
5. Physical activity and weight loss
While diet is the primary driver of weight loss, physical activity plays a complementary role. It enhances caloric expenditure, preserves lean muscle mass, and improves metabolic health.
Physicians should advocate for a combination of aerobic exercise and resistance training, aiming for at least 150 minutes of moderate-intensity exercise per week, coupled with muscle-strengthening activities on two or more days.
6. Addressing common weight loss challenges
- Plateaus: Weight loss plateaus are common and can be frustrating for patients. These occur when the body adapts to a lower calorie intake by reducing metabolic rate. Physicians should reassure patients that this is a normal part of the process and may require adjustments in diet, exercise, or behavioural strategies.
- Nutrient deficiencies: Restrictive diets can lead to nutrient deficiencies. Physicians should monitor patients for signs of deficiencies, particularly in vitamins D and B12, iron, and calcium, and recommend appropriate supplementation if needed.
- Psychosocial factors: Emotional eating, stress, and lack of social support can undermine weight loss efforts. Addressing these issues through counselling, support groups, or referral to a dietitian or psychologist may be necessary.
7. Pharmacotherapy and surgical interventions
For patients with significant obesity or those who have not achieved desired weight loss through lifestyle modifications, pharmacotherapy or bariatric surgery may be indicated. However, these should be considered adjuncts to, not replacements for, diet and behavioural changes. Physicians should ensure that patients understand the importance of continuing lifestyle modifications post-intervention to maintain weight loss.
Case study 1: Transforming weight loss management through personalised nutrition
Patient profile:
- Name: Ms SA
- Age: 45
- Height: 165 cm (5 feet 5 inches)
- Occupation: Office Manager
- Medical history: Type 2 Diabetes, Hypertension, and Obesity
- Current medications: Metformin, Lisinopril
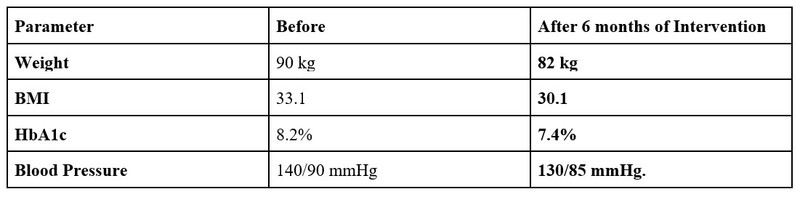 Parameters before and after
Parameters before and after
Presenting issues
The patient presented with difficulty achieving sustainable weight loss despite previous attempts with various diet plans. She reported inconsistent adherence to weight loss recommendations, frequent cravings for high-calorie foods, and a sedentary lifestyle due to long working hours.
Intervention:
1. Personalised nutritional plan
- Dietary changes: Implemented a low-glycemic index diet focusing on whole grains, lean proteins, and healthy fats. Introduced high-fiber foods such as vegetables, legumes, and fruits to improve satiety and stabilise blood sugar levels.
- Portion control: Educated the patient on portion sizes and meal timing to prevent overeating. Suggested using smaller plates and pre-portioned snacks.
2. Behavioural and lifestyle modifications
- Meal planning: Provided a weekly meal plan and cooking tips to help the patient prepare heart-healthy, low-calorie meals. Encouraged batch cooking and healthy recipe modifications to reduce reliance on high-calorie, processed foods.
- Physical activity: Developed a realistic exercise plan starting with 30 minutes of brisk walking daily, gradually increasing to include strength training exercises.
- Stress management: Introduced stress-reducing activities & relaxation techniques such as mindfulness meditation and regular breaks during work to manage stress and emotional eating triggers.
Case Study 2: Addressing overweight and abdominal obesity in a young adult
Patient profile:
- Name: Mr BJ
- Age: 18
- Occupation: Student
- Height: 175 cm (5 feet 9 inches)
- Medical history: Overweight, abdominal obesity, and acanthosis nigricans (dark lines on the neck)
Presenting issues
The patient presented with significant abdominal obesity and dark lines on his neck, which were identified as acanthosis nigricans—a common sign of insulin resistance. He reported difficulty with weight management and an unhealthy diet, characterised by frequent consumption of sugary snacks and beverages.
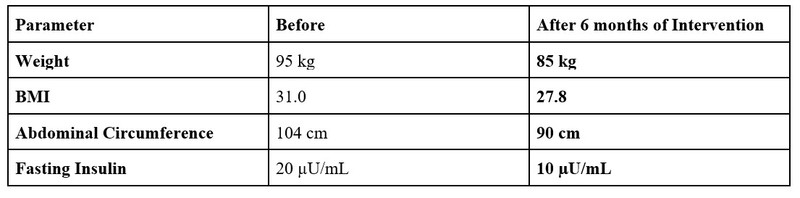
Parameters before and after
Intervention:
1. Personalised nutritional plan
- Dietary changes: Implemented a low-glycemic index diet with whole grains, lean proteins, and vegetables. Reduced intake of sugary snacks and beverages. Increased fibre-rich foods like fruits, vegetables, and legumes.
- Meal timing and portion control: Advised regular meals and snacks to prevent overeating. Educated Alex on portion sizes.
2. Behavioural and lifestyle modifications
- Physical activity: Developed a structured exercise plan with 30 minutes of moderate-intensity exercise five times a week and strength training.
- Screen time management: Suggested reducing screen time and incorporating physical activities or hobbies.
3. Addressing acanthosis nigricans
- Blood sugar monitoring: Recommended screening for insulin resistance and monitoring blood glucose levels.
Conclusion
Weight loss management is a multifaceted process that requires a comprehensive approach. As physicians, understanding the intricacies of diet and nutrition is crucial to guiding patients effectively. By integrating these evidence-based dietary strategies into your practice, you can play a pivotal role in your patients’ weight loss journeys, helping them achieve and maintain a healthier weight, and thereby reducing their risk of chronic disease.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author of this article: Ms Rutambhara Nhawkar is a Clinical Dietician, M. Sc. (Clinical Nutrition & Dietetics), certified diabetes educator and a medical writer from Pune.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries