Diagnosis and Management of Pancreatitis and Pancreatic Disorders
M3 India Newsdesk Jul 15, 2024
The pancreas is a grossly lobulated abdominal organ with both exocrine and endocrine functions. This article provides a comprehensive overview of these conditions, focusing on their diagnosis, management, and the multidisciplinary approach necessary for effective treatment.
Pancreatic disorders: An overview
The primary functions of the pancreas are to secrete the hormones insulin, glucagon, and somatostatin and synthesise digestive enzymes. However, when afflicted by disorders such as pancreatitis or pancreatic cancer, its impact on health can be profound.
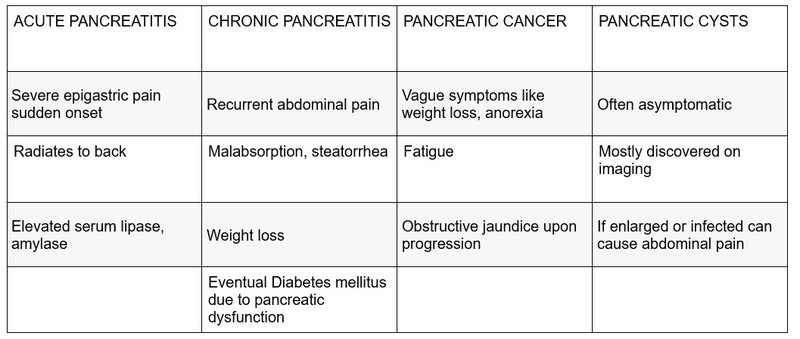
The spectrum of pancreatic disorders encompasses acute pancreatitis, chronic pancreatitis, pancreatic cancer, and pancreatic cysts. Each condition presents unique challenges in diagnosis and management, often requiring specialised care due to the pancreas's complex anatomy and function.
1. Acute Pancreatitis
- Acute pancreatitis AP is a common pancreatic condition caused by inflammation of the pancreas, often triggered by gallstones (40% of cases) or excessive alcohol consumption (30% of cases).
- The condition ranges from mild self-limiting episodes to severe forms that can lead to life-threatening complications such as pancreatic necrosis or systemic inflammatory response syndrome (SIRS) 25% of the time.
- Acute pancreatitis (AP) progresses through two distinct phases: an initial and a prolonged phase.
- The initial phase spans the first week of the illness and is characterised by a systemic inflammatory response. During this period, the clinical severity and treatment approach depend on the type and extent of organ failure.
- The prolonged phase extends beyond the first week and can persist for weeks to months, particularly in severe cases of the disease.
- This phase is distinguished by persistent organ dysfunction and the development of local complications.
- Treatment strategies during the prolonged phase primarily hinge on specific morphological criteria identified through radiographic imaging.
3. Chronic Pancreatitis
Chronic pancreatitis CP develops over time, marked by persistent inflammation and irreversible changes in pancreatic tissue such as fibrosis and ductal strictures. It is commonly associated with chronic alcohol consumption, chronic smoking and a small percentage due to genetic predispositions such as SPINK1, PSSR and CFTR mutations.
The onset of pancreatic fibrogenesis in CP is caused by injury to the interstitial mesenchymal cells, duct cells, and acinar cells depending on the causal factor. CP can lead to pancreatic insufficiency, diabetes mellitus, and an increased risk of pancreatic cancer.
Pathogenesis: Research suggests ethanol consumption is linked to the activation of resident fibroblasts directly bypassing this inflammatory process and causing induction of lithogenic proteins, increasing the viscosity of pancreatic secretions, and forming protein plugs, which cause ductal obstruction and subsequent acinar cell damage and atrophy over time. With each successive pancreatic insult, this pattern of fibrogenesis and atrophy ensues resulting in diminished pancreatic function.
There is evidence linking alcohol consumption and tobacco smoking to an increased risk of CP in people with recurrent pancreatitis and an increased risk of recurrent pancreatitis following an initial episode of AP.
3. Pancreatic cancer
Pancreatic cancer is one of the most aggressive malignancies, often diagnosed at advanced stages due to nonspecific symptoms early in the disease course. It carries a poor prognosis, with surgical resection offering the best chance of long-term survival for localised disease. The most common type is ductal adenocarcinoma.
4. Pancreatic cysts
Pancreatic cysts are fluid-filled sacs within the pancreas, which can be benign or potentially precancerous. They are increasingly detected incidentally on imaging studies performed for other reasons and require careful evaluation to determine the risk of malignancy and the need for intervention.
Clinical presentation
The clinical presentation of pancreatic disorders varies widely but often includes abdominal pain, nausea, vomiting, and in more severe cases, systemic signs of inflammation such as fever and tachycardia.
- Diagnostic evaluation: Accurate diagnosis of pancreatic disorders relies on a combination of clinical evaluation, imaging studies, and laboratory tests:
- Laboratory tests: Serum amylase and lipase levels are crucial for diagnosing acute pancreatitis. Elevated liver function tests may suggest biliary obstruction or pancreatic cancer.
- Imaging studies: Abdominal ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) are essential for visualising pancreatic morphology, identifying gallstones, evaluating pancreatic cysts, and staging pancreatic cancer. Endoscopic Procedures: Endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP) play roles in diagnosing pancreatic cancer, evaluating pancreatic cysts, and providing therapeutic interventions such as stent placement for biliary obstruction.
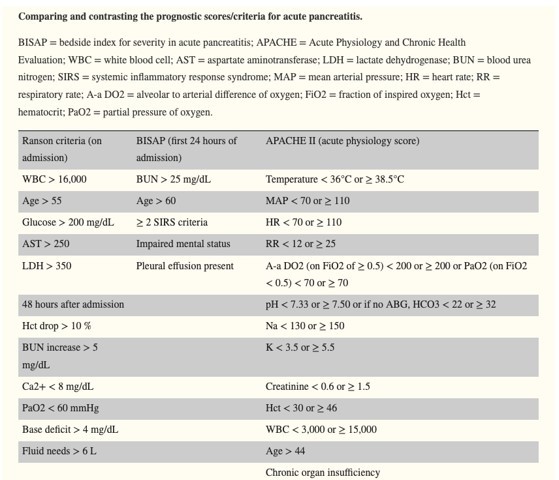
Severity assessment for acute pancreatitis
Severity assessment guides management decisions and predicts outcomes.
Scoring systems like Ranson's criteria or the Acute Physiology and Chronic Health Evaluation II (APACHE II) score help stratify patients into mild, moderate, or severe categories based on clinical and laboratory parameters.
Severe acute pancreatitis requires intensive care monitoring and potential interventions such as drainage of pancreatic necrosis or surgical debridement.
Multidisciplinary approach and long-term care managing pancreatic disorders effectively often necessitates a multidisciplinary approach involving gastroenterologists, surgeons, radiologists, oncologists, dietitians, and specialised nursing staff: Acute Care: Initial management focuses on supportive care, pain control, fluid resuscitation, and addressing underlying causes such as gallstone removal or alcohol cessation.
Chronic management
Long-term management of chronic pancreatitis includes pain management, pancreatic enzyme replacement therapy (PERT) for malabsorption, and management of complications such as diabetes mellitus.
- Surgical intervention: Surgical options range from minimally invasive procedures for drainage of pancreatic pseudocysts to complex pancreaticoduodenectomies for pancreatic cancer.
- Palliative care: In cases of advanced pancreatic cancer, palliative care plays a crucial role in improving quality of life through symptom management and psychological support. Long-term outcomes vary significantly depending on the specific disorder and the stage at diagnosis. While pancreatic cancer often carries a poor prognosis due to its aggressive nature, advancements in surgical techniques and adjuvant therapies offer hope for extended survival in select cases. Chronic pancreatitis, although challenging to manage, can be mitigated with lifestyle modifications and adherence to medical therapies.
In conclusion, the diagnosis and management of pancreatic disorders require a nuanced understanding of their pathophysiology, diligent clinical evaluation, and coordinated multidisciplinary care. Ongoing research into genetic predispositions, biomarkers, and therapeutic targets holds promise for improving outcomes and quality of life for patients affected by these complex conditions.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Akshayaa is a General Practitioner at Sri. Balaji Heart Centre, Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries