Diabetes Management: Recent Guideline Updates by AACE (Part 2)
M3 India Newsdesk May 18, 2023
This article addresses the second part of the American Association of Clinical Endocrinologists (AACE) guidelines which provide recommendations for screening and management of co-morbidities such as cardiovascular disease, hypertension, dyslipidemia, kidney disease, and retinopathy.
Hypertension management in a diabetic patient
As per the recommendation blood pressure (BP) goal for most persons with Type 1 diabetes, Type 2 diabetes, or pre-diabetes is <130/80 mm Hg.
- Lifestyle modification remains the first choice of intervention in patients with hypertension, which includes a healthy diet such as a Mediterranean diet, low sodium intake which can be achieved by a DASH diet, daily physical activity and regular exercise to reduce weight.
- If blood pressure goals are not achieved with lifestyle modifications, the use of antihypertensive pharmacotherapy is recommended to achieve individual blood pressure goals.
- As per recommendation antihypertensive agents should be preferred which helps in prevention or slowing the progression of micro- and macrovascular disease along with reducing BP. The use of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin II receptor blocker (ARB) remains the first choice of anti-hypertensive in diabetic patients for BP control and to delay the progression of Diabetic kidney disease or chronic kidney disease in such patients.
- Use of the combination of either ACEi or ARB along with any of the following agents: calcium channel antagonists, diuretics, alpha-blockers and newer generation beta-blockers is recommended in patients not achieving BP goals with single agents. Mineralocorticoid receptor antagonists are to be considered in cases of resistant hypertension.
Diabetic kidney disease or CKD management in diabetes mellitus
As per recommendation, an annual assessment of serum creatinine and urine albumin-to-creatinine ratio is advised for identifying, staging, and monitoring the progression of Diabetic kidney disease (DKD). Annual assessment post 5 years after diagnosis in persons with type 1 diabetes or at diagnosis in persons with type 2 diabetes.
- Patients with DKD should be counselled about optimal glycemic control, blood pressure control, and lipid control along with smoking cessation to reduce the risk of development and progression of diabetic kidney disease and cardiovascular disease.
- As per recommendation, renin-angiotensin-aldosterone system blockade with an ARB or an ACE inhibitor remains the choice of drug for diabetic patients with micro- or macro albuminuria to reduce the risk of DKD progression.
- A sodium-glucose co-transporter 2 inhibitor (SGLT2i) with proven benefit is recommended as a foundational therapy for persons with type 2 diabetes and DKD with eGFR>20 mL/min/1.73 m2 to reduce the progression of DKD and risk of CVD.
- A glucagon-like peptide-1 receptor agonist (GLP-1 RA) with proven benefit is recommended for persons with T2D and DKD with eGFR >15 mL/min/1.73 m2 for glycemic control and to reduce the risk of ASCVD and progression of albuminuria.
- A non-steroidal mineralocorticoid receptor antagonist like finer enone with proven kidney and CVD benefit is recommended for persons with type 2 diabetes, with an eGFR >25 mL/min/1.73 m2, normal serum potassium concentration, and albuminuria (ACR >30 mg/g) despite a maximum tolerated dose of a renin-angiotensin system inhibitor. Regular monitoring of potassium is advised.
Retinopathy management in a diabetic patient
As per recommendation person with type 2 diabetes and adult–onset type 1 diabetes should have a comprehensive eye examination by an ophthalmologist or optometrist at the time of diagnosis. Subsequent screening can be based on type and duration of diabetes, HbA1c, presence of hypertension, pregnancy and presence of retinopathy.
- As per recommendation a comprehensive eye examination by an ophthalmologist or optometrist for patients with type 1 diabetes should be performed within 5 years of diagnosis in children and adolescents.
- As per recommendation women who are pregnant and have preexisting diabetes should be examined and monitored by an ophthalmologist or optometrist every trimester during pregnancy and in the postpartum period as determined by the severity of retinopathy during pregnancy.
- Persons with greater than mild non-proliferative retinopathy should have an eye examination at least once a year and more frequently as advised by their ophthalmologist. Follow-up with ophthalmologists typically should occur on an annual basis, but persons with diabetes who have had a normal ocular examination may be screened every 2 to 3 years.
- Diabetic patients should be counselled about optimal blood sugar levels, blood pressure, weight, and lipid control to slow the progression of retinopathy.
- Artificial intelligence systems, authorised by the US Food and Drug Administration (FDA) for detecting greater than mild diabetic retinopathy, can be used as an alternative to traditional screening approaches.
Dyslipidemia management in a diabetic patient
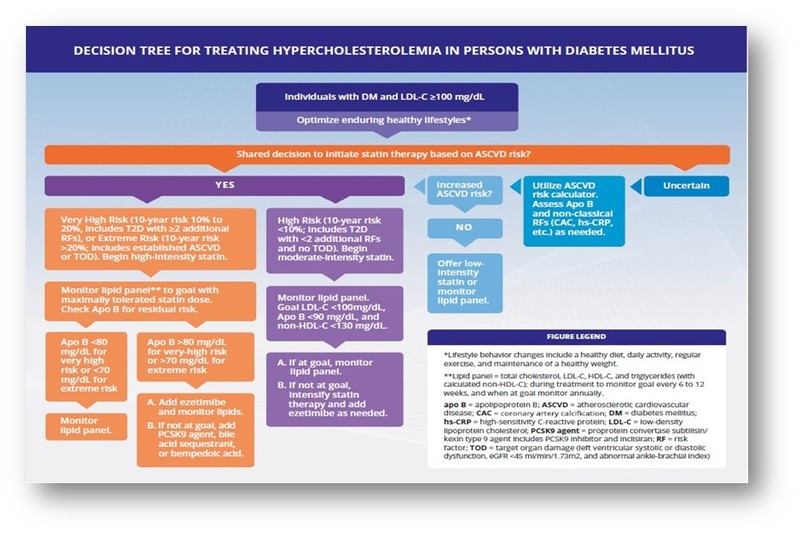
As per recommendation, a lipid panel (fasting or non-fasting) should be checked at diagnosis and annually to assess CVD and metabolic disease risk in persons with pre-diabetes, T1 Diabetes over the age of 40 or type 2 diabetes.
- As per recommendation, therapeutic lifestyle intervention remains the first choice of treatment in prediabetes, type 1 diabetes over the age of 40, or type 2 diabetes with dyslipidemia. It should also include an education session with a registered dietitian or trained physician regarding the importance of weight management, daily physical activity and regular exercise.
- A person with pre-diabetes, T1D over the age of 40, or T2D with less than two traditional risk factors should be assessed with the aid of an ASCVD risk calculator to make a decision regarding the initiation and intensity of lipid-lowering drugs.
- In persons with high ASCVD risk, use a moderate-intensity statin regardless of DM type or status. In persons with very high ASCVD risk (T2D with 2 or more additional traditional ASCVD risk factors such as advancing age, hypertension, chronic kidney disease (CKD) stage 3a, cigarette smoking, family history of premature ASCVD in men <55 y and women <65 y, low high-density lipoprotein cholesterol (HDL-C), or high non-HDL-C), use a high-intensity statin regardless of baseline low-density lipoprotein cholesterol (LDL-C) level. For persons at extreme risk of ASCVD event (current ASCVD or target organ damage), use a high-intensity statin plus other therapies as needed to achieve lipid targets.
- Treatment targets for persons in
- High ASCVD risk categories are LDL-C <100 mg/dL, apolipoprotein B (apo B) <90 mg/dL, and non-HDL-C <130 mg/dL.
- Very high-risk ASCVD categories are LDL-C <70 mg/dL, apo B <80 mg/dL, and non-HDL-C <100 mg/dL.
- Extreme risks of ASCVD include LDL-C <55 mg/dL, apo B <70 mg/dL, and non-HDL-C <90 mg/dL.
- As per recommendation, statins are the initial choice of drug for hypercholesterolemia. Efficacy should be monitored every 6 to 12 wk and the dose of statin should be up-titrated when needed and as tolerated by the patient to achieve LDL-C, apo B, and/or non-HDL-C goals based on individual ASCVD risk. Once lipid targets are achieved, the lipid panels can be monitored less frequently.
- As per recommendation combine ezetimibe with statin therapy when the desired lipid targets are not achieved with a maximally tolerated statin dose. If the lipid targets are not achieved with this combination, the use of proprotein convertase subtilisin/kexin type 9-lowering agent is advised along with statin. Alternatively, the addition of bempedoic acid to the maximally tolerated statin or consider adding icosapent ethyl (in persons with triglycerides 135 to 499 mg/dL) for ASCVD risk reduction.
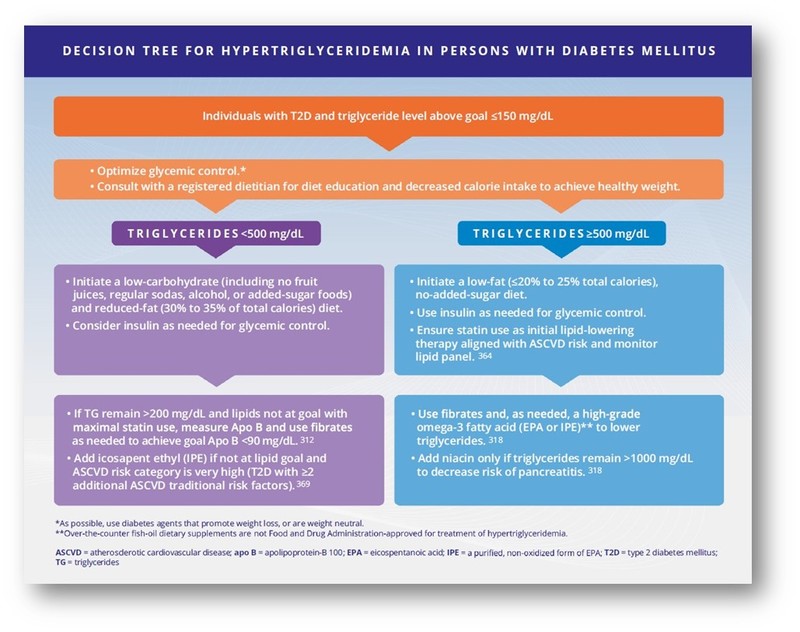
- As per recommendation intensive lifestyle modification and statin therapy remain the choice of management in patients with hypertriglyceridemia who are at high or very high risk of ASCVD. The addition of fibrate or high-dose omega-3 fatty acid is advised in patients not attaining triglyceride concentrations >200 mg/dL and HDL-C <40 mg/dL even after the maximally tolerated statin dose. Icosapent ethyl can be considered in patients with high or very high ASCVD risk.
Neuropathy diagnosis and management in diabetic patients
Diabetic peripheral neuropathy (DPN) is a clinical diagnosis. A comprehensive differential diagnosis should be considered to rule out non-diabetic neuropathies.
- As per recommendation screening for DPN should be done at diagnosis of type 2 diabetes, within 5 years of the diagnosis of type 1 diabetes, and subsequently annually or whenever the patient has symptoms related to neuropathy, by performing a clinical history and physical exam.
- As per recommendation assessments for diabetic neuropathy should include a careful history to assess target symptoms and a combination of at least two of the following:
- Vibration sensation using a 128-Hz tuning fork,
- Pinprick sensation
- Temperature discrimination
- 10-g monofilament testing on the dorsal aspect of the great toe
- Ankle reflexes
- All these assessments should follow the typical diabetic neuropathy pattern, starting distally (the dorsal aspect of the hallux) on both sides and moving proximally until a sensory threshold is identified.
- As per recommendation screening for cardiovascular autonomic neuropathy (CAN) should be considered at diagnosis of type 2 diabetes and at 5 years after the diagnosis of type 1 diabetes, including youth. Screening for CAN should also be considered in the presence of DPN, DKD, two or more Cardiovascular risk factors, hypoglycemia unawareness, high glucose variability, in persons with heart failure (HF), perioperatively, or in individuals presenting with autonomic symptoms.
- Cardiovascular reflex tests like deep breathing, Valsalva, and supine to standing to remain the gold standard and are recommended for assessment of CAN. An easier alternative for screening for CAN indices of heart rate variability derived from electrocardiogram recordings could also be used.
- As per recommendation, diabetic foot exams should be performed at every visit (in person or virtual) to identify deformities and to identify those at risk for late complications such as ulcerations and amputations associated with uncontrolled diabetes.
- To prevent the onset of DPN and CAN in type 1 diabetes, intensive control of glucose is recommended. In type 2 diabetes optimal glucose control, blood pressure control, and lipid control along with lifestyle interventions including a combination of regular aerobic, strengthening, and balance exercises, reduction of sedentary behaviour, and dietary modification aimed at reducing calorie intake and increasing plant-based and polyunsaturated fats are recommended can help in the prevention of DPN and CAN. Lifestyle interventions are effective for DPN and CAN prevention in persons with prediabetes/metabolic syndrome.
- Pharmacological treatment with pregabalin, duloxetine, and capsaicin 8% patch is recommended for the treatment of neuropathic pain due to Diabetes and has received regulatory approval in the United States. Drugs like gabapentin and some tricyclic antidepressants may be as effective to achieve a clinically meaningful reduction in diabetic neuropathic pain. Combining two or more agents from different classes may have enhanced benefits with lower adverse effects and risks than maximising the dose of one medication or using opioids. The use of opioids, including tapentadol or tramadol, is NOT RECOMMENDED due to the high risk of addiction and other complications.
As per recommendation neuromodulatory techniques such as high-frequency spinal cord stimulation and combining pharmacological with non-pharmacological approaches should be considered in those with refractory painful DPN.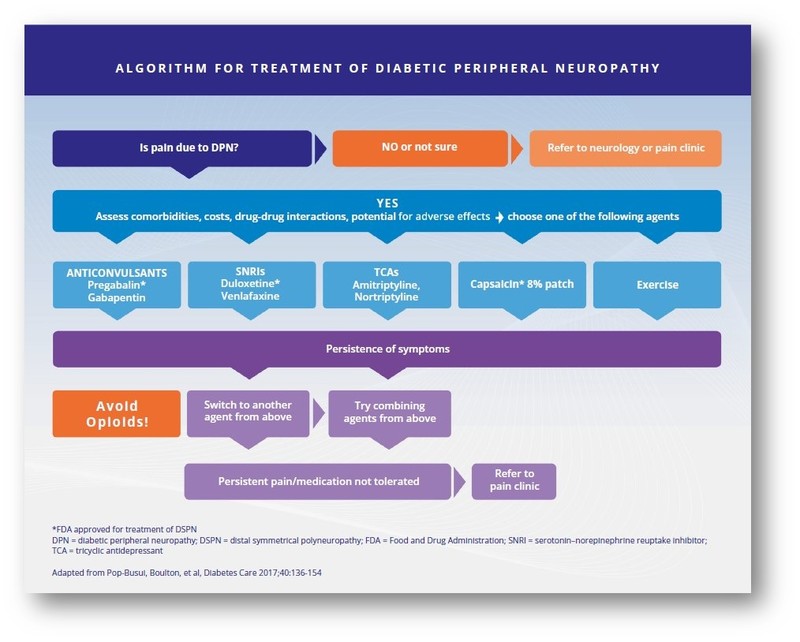
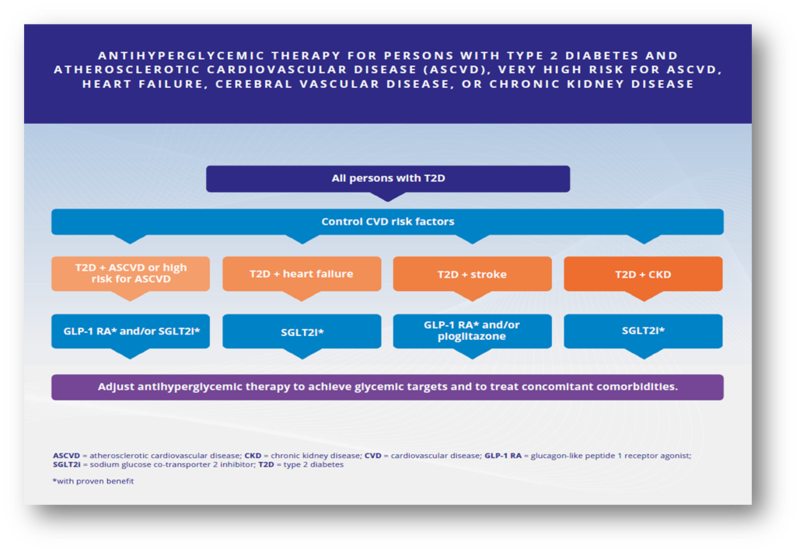
Management of diabetes in high risk for/or with established CVD
As per recommendation patients with type 2 diabetes and established ASCVD or at high risk for ASCVD, the use of GLP-1 RAs with proven CV benefits should be encouraged to reduce the risk of myocardial infarction, stroke, or cardiovascular mortality regardless of other glucose-lowering or CV therapies and independent of HbA1C.
- In patients with type 2 diabetes and established ASCVD or very high ASCVD risk, use SGLT2is with proven CV benefits to reduce the risk of hospitalisation for heart failure, major adverse CV events, or CV death regardless of background glucose-lowering therapy, cardiovascular therapy, or HbA1C.
- As per recommendation in patients with type 2 diabetes and established HF (regardless of ejection fraction, background glucose-lowering or HF therapies, or A1C), use of SGLT2i with proven HF benefits should be encouraged to reduce the risk of hospitalisation for HF or CV death and to improve HF-related symptoms.
- In patients with type 2 diabetes and ASCVD or at high risk for ASCVD, use GLP-1 RAs with proven benefits for a reduction in the risk of stroke. In persons with insulin resistance, prediabetes, or type 2 diabetes and a prior transient ischemic attack (TIA) or stroke, pioglitazone should be considered to reduce the risk of recurrent stroke.

Obesity management in patients with diabetes
The diagnosis and evaluation of obesity/adiposity-based chronic disease ABCD in persons with prediabetes, type 1 or type 2 diabetes should include both anthropometric and clinical components. The anthropometric evaluation should include BMI. Waist circumference (WC) should be measured as a marker of cardiometabolic disease (CMD) risk.
- For most adults, a BMI in the range of 25 to 29.9 kg/m2 is categorised as overweight and BMI >30 kg/m2 is categorised as obese, and waist circumference threshold values are >102 cm for men and >88 cm for women. These values differ for the Asian population.
- The clinical evaluation of persons with both prediabetes, type 1 or type 2 diabetes and obesity should assess the presence and severity of weight-related complications including:
- Cardio-metabolic complications such as dyslipidemia, hypertension, nonalcoholic fatty liver disease (NAFLD)/nonalcoholic steatohepatitis (NASH), CVD, Heart failure, and DKD;
- Biomechanical complications such as obstructive sleep apnea (OSA), osteoarthritis, gastroesophageal reflux disease (GERD), and urinary incontinence;
- Abnormalities involving sex steroids, such as infertility, polycystic ovary syndrome (PCOS), and hypogonadism;
- Impact on psychological disorders and quality of life (QoL).
- As per recommendation patients with type 2 diabetes and obesity should be counselled for weight loss intervention which will improve glycemic control as well as complications related to obesity. The target for weight loss should be >5% to >10% of baseline body weight. This can be achieved with lifestyle interventions, a calorie-deficit diet, daily physical activity, regular exercise for >150 minutes a week and behavioural health practices.
- The Mediterranean, low-fat, low-carbohydrate, very low-carbohydrate, vegetarian, vegan, and DASH diets are recommended, safe, and effective for short-term weight loss.
- Only the Mediterranean diet has evidence of long-term risk reduction for CVD events and mortality amongst all other diets.
- Patients with type 2 diabetes and obesity with BMI >27 kg/m2 should be treated with diabetic medications associated with weight loss like GLP-1 RAs and SGLT2 inhibitors. In addition, for persons with prediabetes, type1 or type2 diabetes who have obesity, consider FDA-approved weight-loss medications as an adjunct to lifestyle intervention to achieve lowering of HbA1C, reduction of CVD risk factors, treatment or prevention of other ABCD complications, and improvement in quality of life.
- A person with a BMI >35 kg/m2 and one or more severe obesity-related complications remediable by weight loss, including type 2 diabetes, high risk for diabetes (insulin resistance, prediabetes, and/or metabolic syndrome), poorly controlled hypertension, NAFLD/NASH, obstructive sleep apnea, osteoarthritis of the knee or hip, and urinary stress incontinence, should be considered for a bariatric procedure.
- As per recommendation, diabetic patients with a BMI of 30 to 34.9 kg/m2 with inadequate glycemic control despite optimal lifestyle intervention and medications should be considered for a bariatric procedure.
Click here to read part 1- Recent Updates in Diabetes Practice: AACE Guidelines
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist, physician and an obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries