CSI Dyslipidemia Management Guidelines for Indian Population
M3 India Newsdesk May 28, 2024
The guidelines by the Cardiovascular Society of India outline the assessment and treatment of dyslipidemia in India, emphasising lifestyle changes, pharmacological interventions, and considerations for specific conditions to reduce the high CAD incidence.
In India, the prevalence of dyslipidemia and Coronary Artery Disease (CAD) has been steadily increasing over the past few decades, largely due to changes in lifestyle, dietary habits, urbanisation, and an ageing population. CAD, which is often a consequence of long-standing dyslipidemia among other risk factors, is a leading cause of morbidity and mortality in India.
The Indian population is particularly predisposed to CAD due to a combination of genetic predisposition, lifestyle factors (such as unhealthy diet, lack of physical activity, and smoking), and increasing rates of obesity and diabetes. These guidelines are important for our Indian population when compared to the world population as we have a propensity to develop CAD 10 years earlier, and we have higher ASCVD risk factors at a young age like hypertension, diabetes, tobacco (chewing and smoking), metabolic syndrome (~40 % population with central obesity). Indian population have atherogenic dyslipidemia i.e. high triglycerides, low HDL, and high LDL. Considering genetic causes we have familial hypercholesterolemia in around 15 % of the young CAD as compared to 10% in the Western world, and lipoprotein a is in around 25% of the general population.
The Clinical Practice Guidelines for Dyslipidemia Management, developed by the Cardiovascular Society of India (CSI), aim to provide evidence-based recommendations for the assessment and treatment of dyslipidemia, a condition characterised by abnormal levels of cholesterol and triglycerides in the blood. Here's an executive summary of the guidelines:
Assessment of lipid profile
Measurement of non-fasting lipid profile for risk estimation and guiding treatment is recommended. Measurement of lipid profile in emergency and clinics can help in early estimation of CAD risk and rapid initiation of lipid-lowering treatment.
Risk stratification
Patients should be stratified into different risk categories based on their lipid levels and other cardiovascular risk factors to guide lipid-lowering therapy and to identify goals. Risk categories include low, moderate, high, and very high risk.
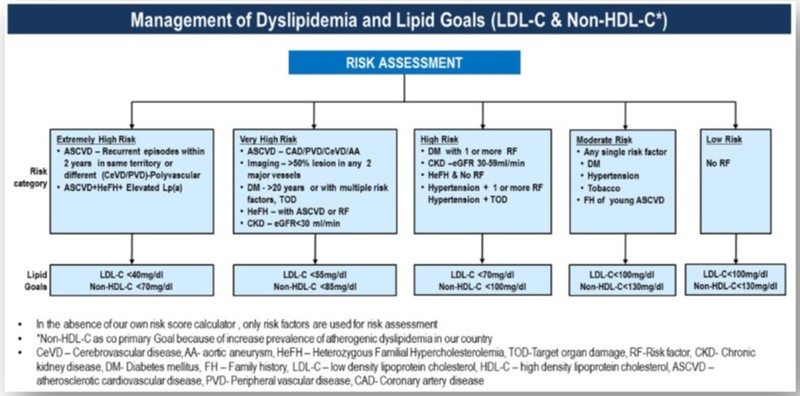
Cardiovascular risk estimation and lipid management goals
Lifestyle modifications
Lifestyle modifications should be recommended as the first-line approach for all patients with dyslipidemia. This includes dietary changes, regular physical activity, smoking cessation, and weight management.
Moderate physical activity should ideally be performed daily or at least 5 days a week to achieve a target of 150 min/week, resistance training should be included thrice per week.
Pharmacological treatment
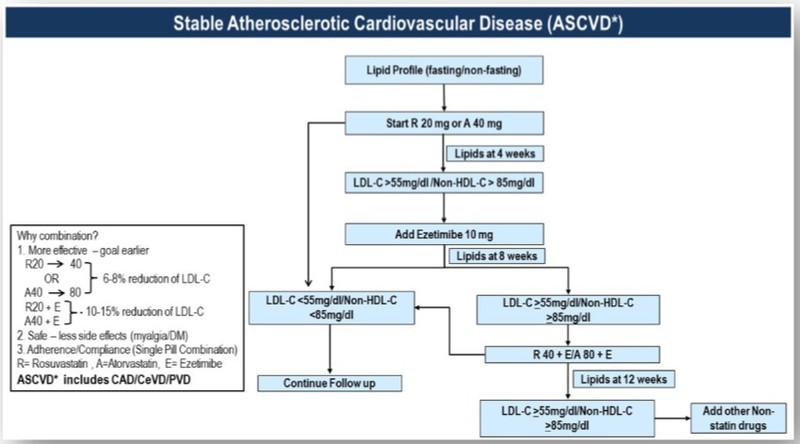
A proven concept in LDL cholesterol management in ACS is to ‘hit hard and hit early’ with a combination of lipid-lowering therapy starting with statins as the first line of the drug.
Pharmacological therapy is recommended in addition to lifestyle modifications for patients with persistent dyslipidemia, especially those at moderate to high risk. Statins are the first-line pharmacotherapy for reducing LDL cholesterol levels.
Statins have proven protective effects in all clinical situations: primary prevention, secondary prevention, following revascularisation, diabetes and patients with HFeH.
Observational studies have indicated that South Asians and Indians tend to be hyper-responsive to statins, often needing lower doses to attain similar therapeutic effects. Additionally, this population may be more prone to experiencing adverse effects from statins. Rosuvastatin (water soluble) and atorvastatin (fat-soluble) are recognised as the most potent statins, with lower doses of these medications categorised as moderate-intensity statins.
Statins have been associated with muscle and liver toxicity in some populations. This should be promptly detected and treated. Reducing the dosage, temporarily discontinuing with cautious reintroduction, or transitioning to a less potent statin could be beneficial.
Commonly available statins in India and daily dose according to intensity of treatment.
| Drug | High Intensity | Moderate intensity | Low intensity |
|---|---|---|---|
| Atorvastatin | 40-80 mg | 10-20 mg | 5 mg |
| Rosuvastatin | 20-40 mg | 5-10 mg | - |
| Pitavastatin | - | 2-4 mg | 1 mg |
Other lipid-lowering agents, such as ezetimibe, bile acid sequestrants, fibrates, and PCSK9 inhibitors, and inclisiran may be considered as adjunctive therapy in certain cases.
It is recommended to add another non-statin drug if an LDL cholesterol target of <55 mg/dl is not achieved at 4 weeks after initiation of Statins: choices are bempedoic acid, PCSK9 inhibitors or inclisiran.
Ezetimibe may be used alone (15 % reduction in LDL cholesterol) or in combination with Bempedoic acid (40 % reduction in LDL cholesterol) in statin-intolerant patients. It is recommended for use either alone or in combination with ezetimibe in patients who cannot tolerate statins. When used alone, bempedoic acid decreases LDL cholesterol by 25%.
Inclisiran is a long-acting small interfering RNA (siRNA) that blocks the transcription of PCSK9. This results in a decrease in PCSK9 generation in hepatocytes and an increase in LDL receptor expression in the liver cell membrane leading to about 50 % reduction in serum LDL cholesterol levels. Inclisiran is administered subcutaneously twice a year and has the potential for better compliance and it causes less LDL-C variability. Inclisiran therapy is associated with a 24 % lower rate of major adverse cardiovascular events with no increase in unwanted side events.
PCSK9 inhibitors reduce LDL receptor (LDLR) clearance and increase hepatic LDLR density which results in increased hepatic uptake and lowering of LDL cholesterol. Evolocumab and alirocumab, both PCSK9 inhibitors, have been approved for clinical use. Evolocumab is available in India. PCSK9 inhibitors can reduce LDL cholesterol by 50-60 %. The dose is 140 mg every 2 weeks or 420 mg once a month given subcutaneously.
Currently, they are used to reduce LDL cholesterol below 70 mg/dl in high-risk patients on maximally tolerated doses of statins and/ or ezetimibe who fail to reach targets. PCSK9 inhibitors are very efficacious but expensive. They should be used in those who are most likely to benefit from a very high ASCVD risk population.
Lipid management in chronic coronary syndromes
Fenofibrate: In patients with mild to moderate hypertriglyceridemia (TG 150- 499 mg/dl), there is no role for fibric acid derivatives. In those with diabetes (>40 years) or ASCVD, IPE may be considered if TG remains high after lifestyle measures and control of diabetes. The most definite indication of fenofibrate monotherapy is fasting serum triglyceride >500 mg/dl, primarily to reduce the risk of acute pancreatitis.
Fish oils (eicosapentaenoic acid EPA, docosahexaenoic acid DHA) reduce serum triglycerides by about 25 %. They may mildly increase LDL cholesterol levels.
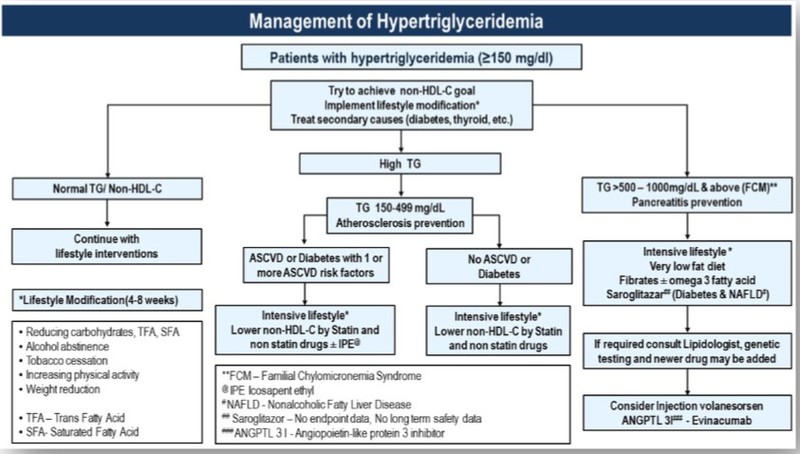
Management of hypertriglyceridemia
Special considerations
Management of dyslipidemia in pregnancy and breastfeeding
During pregnancy, it's common for serum triglycerides and total cholesterol levels to rise. The primary approach to managing these elevated levels in pregnant women involves dietary interventions. Omega 3 fatty acids and bile acid sequestrants are safe but only moderately effective. Statins are contraindicated in pregnancy and breastfeeding.
Liver disease
Statins are the primary treatment for dyslipidemia in metabolic dysfunction-associated steatotic liver disease (MASLD). Mild elevation (up to 3 fold) of liver enzymes is not a contraindication for statin treatment. However, they are contraindicated in decompensated cirrhosis or acute liver failure.
Drug interactions must be considered when prescribing statins to CLD patients particularly when given with antiviral drugs for hepatitis B and C.
Chronic kidney diseases
About 50% of cases of chronic kidney disease have been associated with CVD which makes a multipronged approach a necessity to reduce mortality in such patients. Extensive clinical trials have demonstrated that statins lower the risk of all-cause mortality and cardiovascular (CV) events among individuals with chronic kidney disease (CKD).
Lipid-lowering therapy with a statin with or without ezetimibe is recommended in patients with eGFR <60 ml/min/1.73 m2 and also in those with a preserved GFR but who have an increased urinary albumin-to-creatinine ratio (>3 mg/mmol) for at least 3 months.
For most hemodialysis patients without evidence of ASCVD, it's recommended not to discontinue statin treatment. Those who were already using statins, ezetimibe, or a combination of both before starting dialysis should contemplate maintaining these medications, particularly if they have ASCVD.
Combining fibrates with statins in CKD patients is discouraged, and using ezetimibe alone is not advisable. Bempedoic acid is safe for those with mild to moderate kidney impairment, and dosage adjustments aren't required for such patients.
Dyslipidemia in children
Pharmacotherapy is best avoided in children less than 10 years of age except in the presence of severe primary hyperlipidaemia, familial hypercholesterolemia or multiple risk factors.
Statins and fibrates are the primary medications used to treat high cholesterol levels (hypercholesterolemia) and high triglyceride levels (hypertriglyceridemia), respectively. Monitoring of liver functions, creatine kinase, and lipid profile should be performed following 1 month of therapy and every 36 months thereafter.
Children aged 10 years and older can receive ezetimibe as a medication. A phase-4 study in India, which included children 12-18 years reported that PCSK9 inhibitor- evolocumab was safe and well tolerated.
Familial hypercholesterolemia
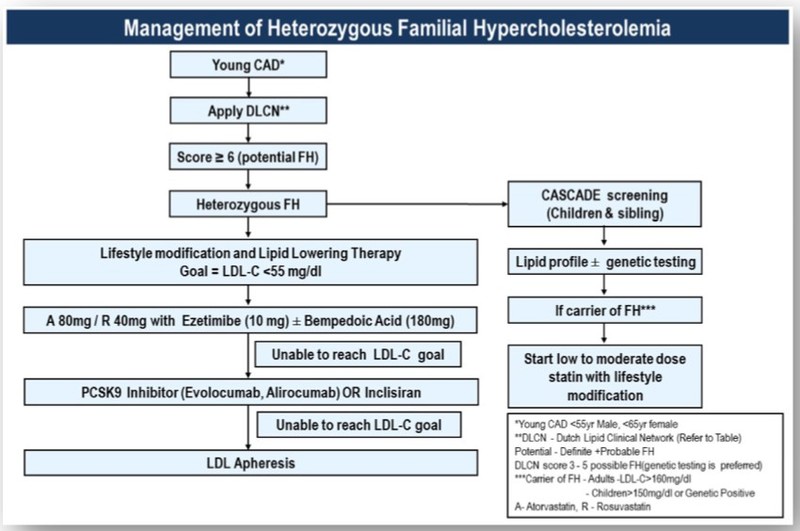
Familial hypercholesterolemia (FH) is a genetic disorder characterised by high levels of low-density lipoprotein (LDL) cholesterol from birth, leading to an increased risk of cardiovascular diseases at an early age. Studies have shown that FH exists in the Indian population, although it may be underdiagnosed due to limited awareness and screening programs. Given the diverse genetic makeup of India's population, the specific genetic mutations associated with FH may differ from those in other populations.
It's essential for healthcare providers in India to consider FH as a potential diagnosis in individuals with early-onset cardiovascular diseases or markedly elevated cholesterol levels, particularly if there is a family history of similar conditions. Early detection through genetic testing and lipid screening can help in the management and prevention of complications associated with FH.
These guidelines provide a comprehensive framework for the assessment and management of dyslipidemia, with a focus on reducing cardiovascular risk and improving patient outcomes. Healthcare providers should use these recommendations in conjunction with clinical judgment and patient preferences to deliver optimal care to manage dyslipidemia in the Indian population.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist, physician and an obesity specialist at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries