Commonly encountered chest/lung CT scan signs and their clinical relevance: Dr. Jyotsna Joshi & Dr. Unnati Desai
M3 India Newsdesk Apr 16, 2020
Dr. Jyotsna Joshi and Dr. Unnati Desai summarise common chest computed tomography findings to help aid in diagnosis of common lung disorders, infections, and malignancies.
For our comprehensive coverage and latest updates on COVID-19 click here.
 With the advent of the computed tomography (CT) in respiratory medicine, a greater delineation of the respiratory structures has been possible in the two dimensional space. The various CT techniques used by pulmonologists include the high resolution computed tomography (HRCT) thorax with expiratory scans, contrast enhanced CT (CECT) thorax, CT thorax, CT pulmonary angiography (CTPA) and rarely a CT aortography/angiography.
With the advent of the computed tomography (CT) in respiratory medicine, a greater delineation of the respiratory structures has been possible in the two dimensional space. The various CT techniques used by pulmonologists include the high resolution computed tomography (HRCT) thorax with expiratory scans, contrast enhanced CT (CECT) thorax, CT thorax, CT pulmonary angiography (CTPA) and rarely a CT aortography/angiography.
The HRCT enhances image resolution using a narrow slice width (1 to 2mm), high spatial resolution image reconstruction algorithm and with minimised field of vision to visualise the minutest of the lung parenchymal details. This modality is best for imaging in airway, parenchymal and interstitial lung diseases. HRCT thorax should mandatorily have expiratory scan study as a part of it.
The mediastinum and pleural involvement is however best studied using a CECT thorax. In cases where a contrast cannot be instituted a plain CT thorax may be used. Special CT techniques like CTPA are used for pulmonary thromboembolism and CT aortography/angiography for pulmonary arteriovenous malformations and pulmonary sequestration.
Structures visible on HRCT and CECT include the bronchi (till the 8th gen), pulmonary artery, pulmonary vein, interlobular septa, fissures, lymph nodes, secondary pulmonary lobule, mediastinum and pleura. Structures not visible on CT are lymphatic vessels, acini, alveoli, capillary vessels, visceral pleura. The common chest CT signs are explained in chronology of the pathological involvement further.
Airway disorders
Emphysema
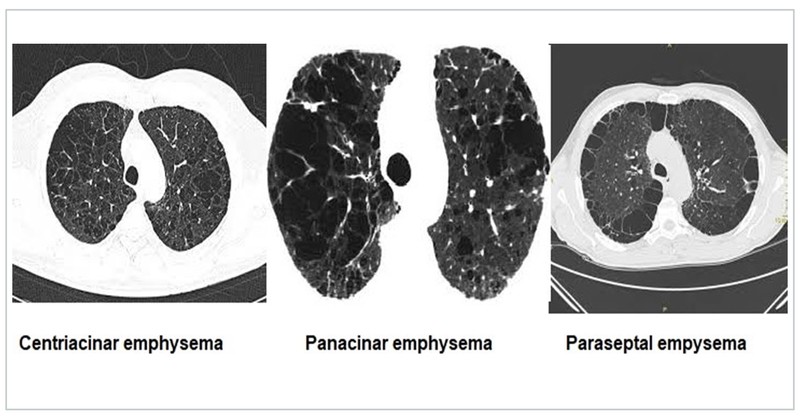
Emphysema is the abnormal permanent dilatation of the airspaces distal to the terminal bronchioles with destruction of the alveolar wall. It is of three types- centriacinar, panacinar, and paraseptal.
- Centriacinar emphysema affects the proximal respiratory bronchioles in the upper lobe seen in smoker COPD.
- Panacinar emphysema affects the entire secondary pulmonary lobule and the entire lung observed in alpha 1 anti-trypsin deficiency.
- Paraseptal emphysema affects the peripheral part of secondary pulmonary lobule adjacent to the pleura and seen around old scars.
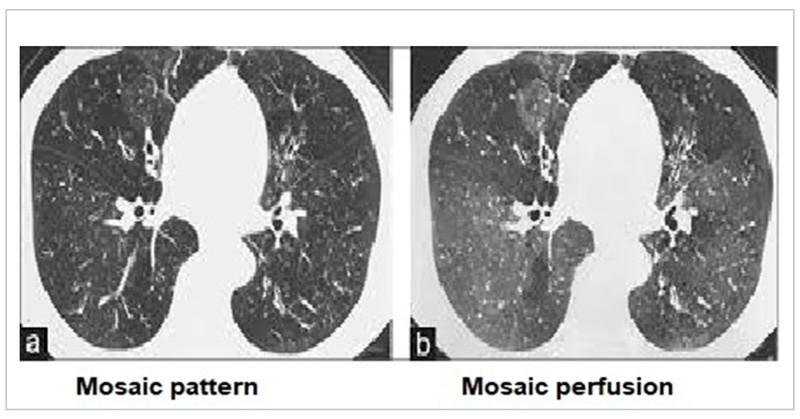
Mosaic attenuation/pattern and mosaic perfusion
Mosaic attenuation is defined as heterogeneous areas of differing lung attenuation. This is the result of diverse causes that include diseases of the small airways, pulmonary vasculature, alveoli, and interstitium, alone or in combination. Mosaic perfusion is the exaggeration of the mosaic attenuation pattern on expiratory scans. It represents air trapping and small airway disease which could be due to obliterative bronchiolitis (OB), COPD, asthma, and interstitial lung diseases (ILD) like hypersensitivity pneumonitis.
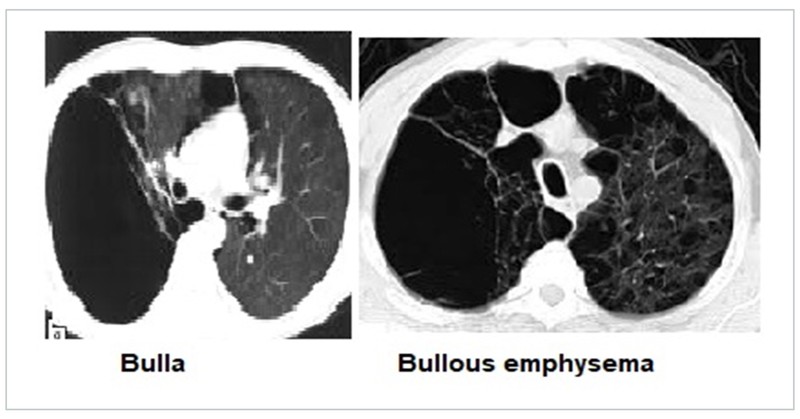
Bleb, cyst, bulla and bullous emphysema
These CT findings are often associated with airway disorders and otherwise. A pulmonary bleb is a small thin walled sub pleural air containing space in the visceral pleura. It may be associated with primary spontaneous pneumothoraces. They may be idiopathic in nature or due to inherited causes like elastin deficiency, Marfan’s syndrome etc.
A pulmonary cyst is a round, thin-walled, parenchymal lucency with a well-defined interface with normal lung. Cysts may be solitary or multiple, idiopathic or associated with airway disorders, ILD, ILD mimics like histiocytosis X and lymphangioleiomyomatosis and cystic lung disease. Pulmonary bulla is a localised region of emphysema with no discernible wall which measures more than 1 or 2 cm in diameter. Bullae may be seen in COPD. When multiple bullae are associated with normal intervening lung parenchyma it is called as bullous lung disease. When multiple bullae are associated with emphysematous lung parenchyma it is labelled as bullous emphysema.

Bronchiectasis
Bronchiectasis, an irreversible abnormal dilatation of the bronchial tree is associated with classical CT findings. Bronchiectasis has varied inherited and acquired causes. CT often helps in diagnosis of 40 to 50% cases of bronchiectasis which is not appreciated on a routine chest X ray.
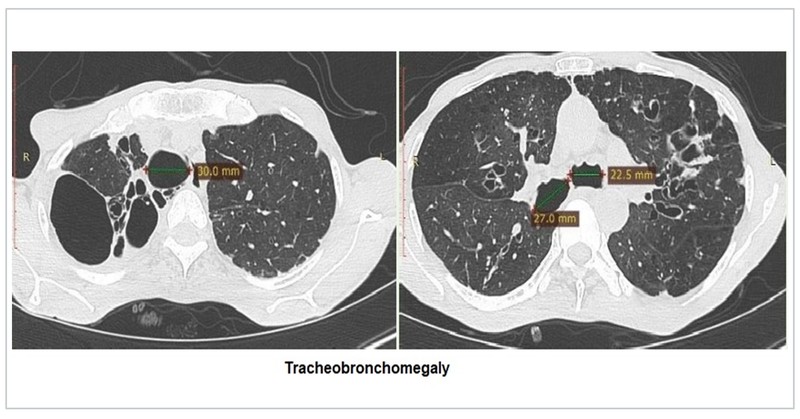
On the basis of CT types; bronchiectasis is classified as cystic, cylindrical and varicose. The signet ring sign, diagnostic of bronchiectasis is due to the dilated bronchus and accompanying pulmonary artery branch seen in cross-section resembling a signet ring. The bronchus and artery should be the same size normally. Tram-track sign denotes the thickened non-tapering (parallel) walls of cylindrical bronchiectasis. Syndromes associated with bronchiectasis may demonstrate tracheobronchomegaly (Mounier Kuhn) and tracheal diverticuli.


Parenchymal diseases
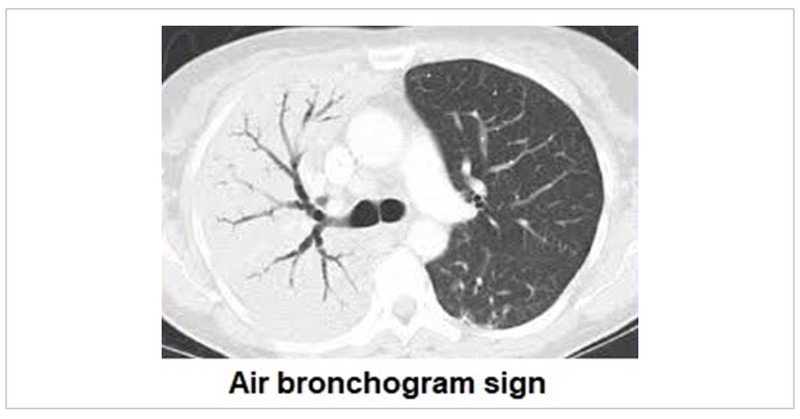
Air bronchogram sign
Air bronchogram sign is a classical CT sign of lung consolidation which could be of numerous aetiologies. The patent airways can be seen thorough the opacified lung parenchyma.
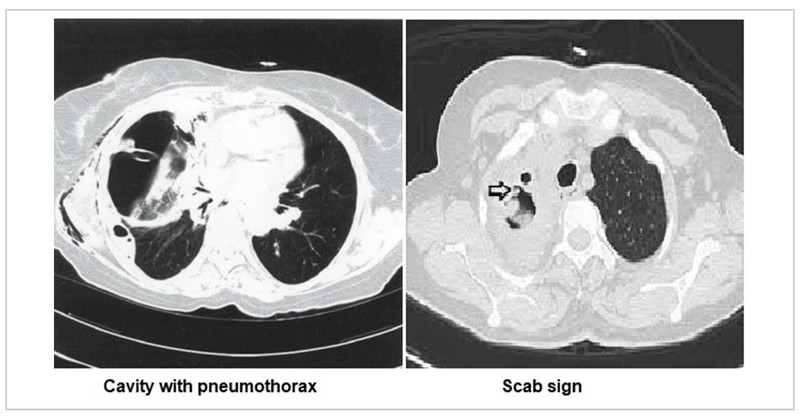
Pulmonary cavity and scab sign
Pulmonary cavity is a thick-walled, air-filled space with or without a fluid level associated with a nodule, mass or consolidation. The spectrum of diseases causing a cavity ranges from infectious, inflammatory, malignant and benign disease processes. While most cavities may be visible on a chest X-ray, cavities that are retrocardiac and apical in nature may be difficult to visualise on a chest radiograph. The cavity may be associated with complications like pneumothorax and hydropneumothorax due to its rupture. The scab sign is characterised by a focal irregular/spiky cavity wall thickening, correlating pathologically with a fibrinopurulent mass and/or blood crust and clinically indicating the site and predisposition to haemoptysis in cavitary pulmonary aspergillosis.
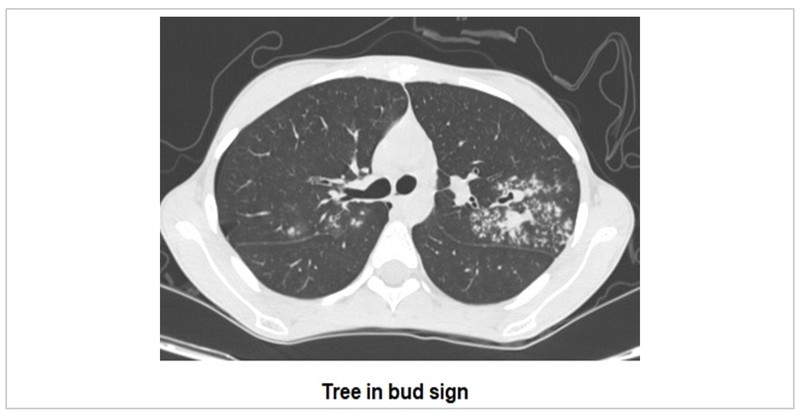
Tree in bud sign
Tree-in-bud sign suggests multiple areas of centrilobular nodules with a linear branching pattern. Initially described in patients with endobronchial tuberculosis, it is now recognised in a large number of conditions again ranging from infections, inflammations, vasculitis to malignancies.
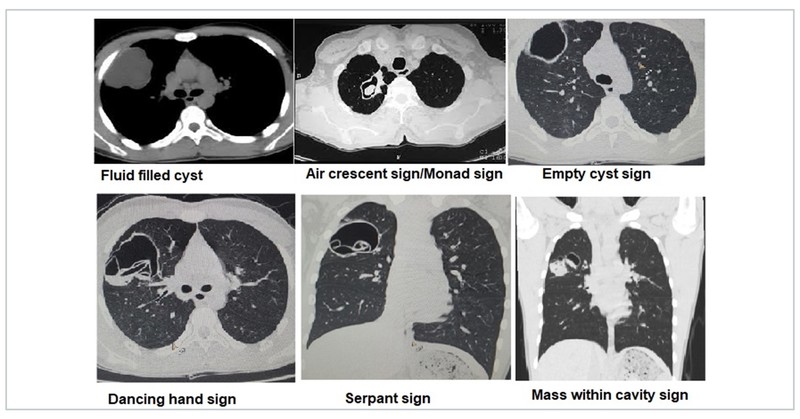
Hydatid cyst
Hydatid cyst has been associated with various CT signs. An unruptured hydatid cyst may appear as a fluid filled cyst. Post rupture or aspiration the hydatid cyst can appear as air crescent sign, water lily sign/Camalote sign, crumpled membrane sign/dancing hand sign, empty cyst sign, serpant sign, or mass within cavity sign.
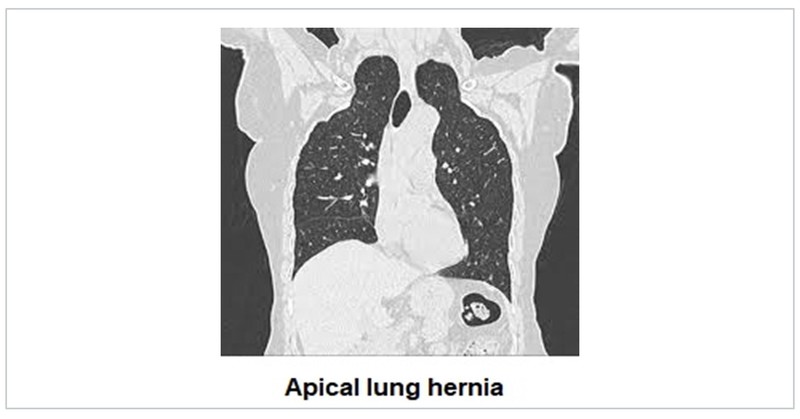
Fissures and anatomical variations
The fissures can be normally seen on the CT thorax. The azygous lobe and fissure may be seen in some. Rarely the lung may herniate through the apex and appear as reducible anterior neck swellings diagnosed as apical lung hernia.
Fallen lung sign, Swiss cheese sign, collar sign
Trauma to lung presents on the CT thorax with common signs like consolidation, infarction, cyst, pneumothorax, pneumomediastinum, subcutaneous emphysema, and fractured ribs. The fallen lung sign describes the appearance of collapsed lung away from the mediastinum encountered with tracheobronchial injury (in particular those >2 cm away from the carina). The Swiss cheese sign has been used for the appearance on CT of fluid-containing pneumatoceles, that typically occur following pulmonary lacerations. The collar sign is suggestive of a diaphragmatic laceration and the CT shows constriction of herniated abdominal content (stomach/intestine) at the site of the diaphragmatic tear to differentiate it from diaphragmatic eventration.

Interstitial lung diseases(ILD)
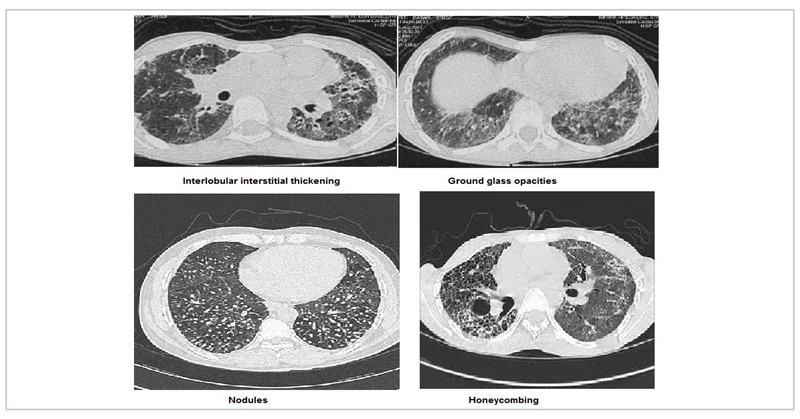
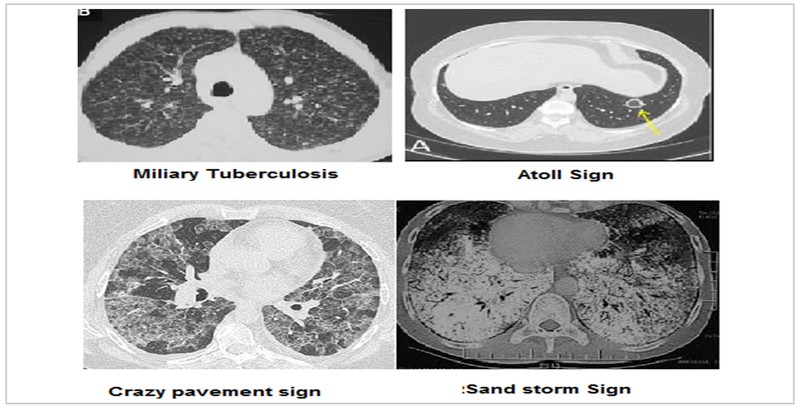
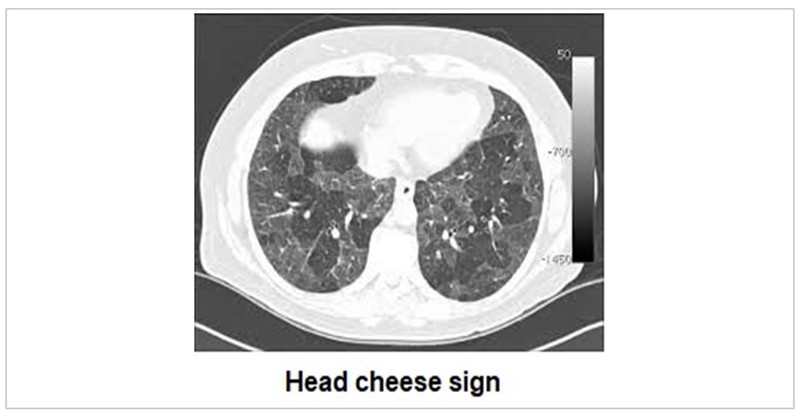
HRCT in ILD is an exhaustive topic in itself. ILD are characterised by interlobular interstitial septal thickening, honeycombing, ground glass opacification and nodules. Idiopathic interstitial pneumonia (IIP) have varied characteristic distribution. Atoll sign is defined as central ground-glass opacity surrounded by denser consolidation and is seen in COP. Sarcoidosis is characterised by fissural nodules and may cause tracheal nodularity. Miliary mottling with randomly scattered nodules in miliary tuberculosis, crazy pavement sign i.e appearance of ground-glass opacity with superimposed interlobular septal thickening and intralobular septal thickening, seen in pulmonary alveolar proteinosis and sand storm sign in pulmonary microlithiasis are some ILD mimics with characteristic CT pattern. The Head Cheese sign consists of juxta-positioning of distinct radiographic areas of low, normal, high attenuation is seen in sub-acute hypersensitivity pneumonitis, sarcoidosis and atypical mycoplasma pneumonias.
Lung malignancy
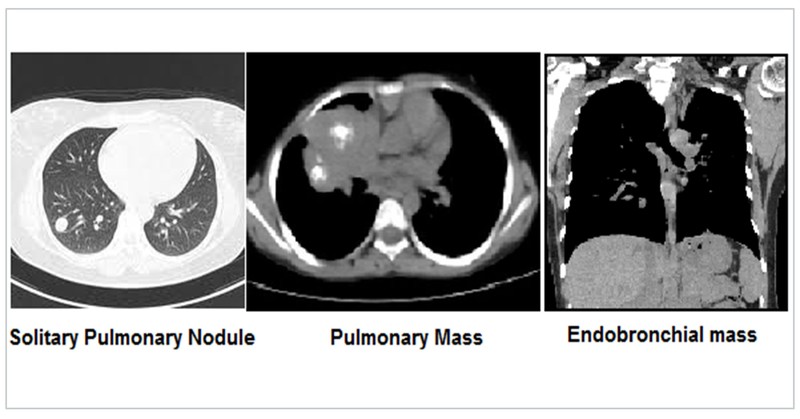
Bronchogenic carcinoma in early stages may present as a solitary pulmonary nodule (SPN) defined as a discrete, well-emarginated, rounded opacity less than or equal to 3 cm in diameter that is completely surrounded by lung parenchyma, does not touch the hilum or mediastinum, and is not associated with adenopathy, atelectasis, or pleural effusion.
Lung malignancy may also present as a pulmonary mass which are larger than SPN. SPN and masses are described as per size, shape, enhancement, boundaries, calcification, satellite lesions, other lobe, opposite lung, rib, lymph node and pleural involvement. Endobronchial involvement results in a positive bronchus sign. Multiple metastases from a distant malignancy to the lung presents as classical cannon ball metastasis.
Pleura
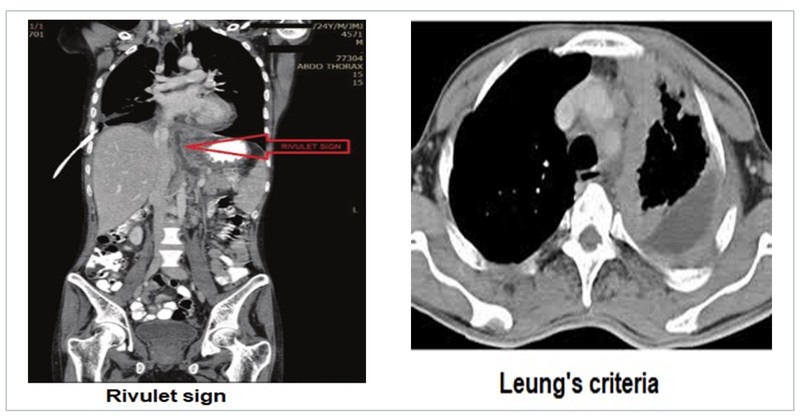
Pleural diseases are often diagnosed with the help of chest radiographs. However, CECT thorax can help further in detailing the anatomy of the pleura often giving a clue to the aetiological diagnosis. The comet tail sign results due to trapping of lung parenchyma in the two layers of pleura during resolution of a pleural effusion. The split pleura sign is a sign of empyema. A pancreatic pleural fistula is described by the rivulet sign.
Pleural plaques and there distribution may be more evident on the CT. Pleural involvement in primary or metastatic lung malignancy is observed and described as per Leung's criteria, which states that any of the following four features of pleural thickening is suggestive of malignant pleural disease:
- Circumferential pleural thickening
- Nodular pleural thickening
- Parietal pleural thickening greater than 1 cm
- Mediastinal pleural involvement
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries