Basics of Cancer Genetics
M3 India Newsdesk Dec 04, 2024
This article is the first in a series that will delve into cancer genetics followed by decoding hereditary cancers, common cancer syndromes, the importance of genetic testing, and much more.
Cancer is a complex disease characterised by uncontrolled cell growth and division, often triggered by genetic mutations. These mutations disrupt the normal functioning of genes responsible for regulating cell growth, DNA repair, and apoptosis (programmed cell death).
Cancer genetics is the field dedicated to understanding these genetic changes and their role in the development and progression of cancer.
The cellular and genetic foundation
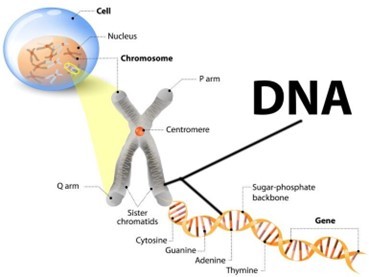
- The cell is the fundamental unit of the human body, housing the nucleus, which contains DNA. DNA, in turn, forms compact structures called chromosomes.
- The human genome consists of 23 pairs of chromosomes. A gene is a unit of DNA that codes for specific proteins or functions, with regions called exons (coding) and introns (non-coding).
- During cell division, maintaining DNA sequence integrity is critical. While DNA replication is highly accurate, occasional errors occur.
- Specialised cellular mechanisms repair these errors before the next cell division. If errors remain unrepaired, they may lead to mutations, which can contribute to cancer development.
Types of cancer-related genes
1. Oncogenes
- Derived from normal genes (proto-oncogenes), oncogenes promote cell growth when mutated or overexpressed.
- Example: HER2 in breast cancer and RAS in various cancers.
2. Tumour suppressor genes
- These genes regulate cell growth, promote DNA repair, and initiate apoptosis.
- Example: TP53, the "guardian of the genome," prevents the proliferation of damaged cells. Mutations in TP53 are linked to many cancers.
3. DNA repair genes
Mutations in these genes increase the risk of further mutations and cancer.
Types of genetic variants in cancer
1. Germline variants
Present in reproductive cells (sperm or egg), these mutations are found in every cell of the body and can be inherited.
2. Somatic (Acquired) variants
It occurs during or before tumour development and is not present in the germline.
Recognising genetic or hereditary cancer
Cancer may be hereditary or genetic if:
1. Family history
Multiple family members are diagnosed with the same or related types of cancer.
2. Germline mutation detection
A germline mutation has been identified in the patient or their family.
Even without a family history, hereditary cancer can be suspected if:
- Cancer develops at an unusually young age.
- Paired organs are affected.
- There are multiple primary cancers in a single individual.
- Features of a hereditary cancer predisposition syndrome are present.
Specific cancer types include:
- Triple-negative breast cancer: High-grade serous ovarian carcinoma
- Colorectal cancer with MSI-high: Medullary thyroid carcinoma, retinoblastoma, neurofibromatosis, brain tumours, etc.
Epigenetics in cancer
While mutations are central to cancer, epigenetic changes also play a significant role.
What is epigenetics?
Epigenetics involves modifications that regulate gene activity without altering the DNA sequence. These changes act as "switches" or "dimmers," controlling gene expression.
Key epigenetic mechanisms
1. DNA methylation
The addition of methyl groups to cytosines in CpG islands often silences genes.
2. Histone modifications
Alterations like acetylation or methylation affect how tightly DNA is packed, influencing gene expression.
3. Non-coding RNAs
Molecules like microRNAs regulate gene expression post-transcriptionally by degrading mRNA or blocking translation.
Epigenetics in hereditary cancers
1. Tumour suppressor gene silencing
Hypermethylation of promoters (e.g., MLH1 in Lynch syndrome) inactivates protective genes.
2. Oncogene activation
Loss of epigenetic control can activate oncogenes, driving cancer progression.
3. The "second hit" in the two-hit hypothesis
Inherited mutations can be complemented by epigenetic changes, inactivating both copies of a tumour suppressor gene.
Conclusion
Cancer genetics is a dynamic field, unravelling the interplay between genetic mutations and epigenetic alterations in cancer development. Understanding these mechanisms paves the way for personalised medicine, targeted therapies, and better prevention strategies.
Future articles in this series will explore hereditary cancer syndromes, genetic testing, and emerging advancements in cancer genetics.
"The study of cancer genetics is not just about unravelling the mysteries of disease; it's about understanding the essence of life and how we can protect it."
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Archi Rungta, BDS, Currently pursuing a PG Diploma in Cancer Genetics and Genetic Counselling from Tata Memorial Hospital, Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries