A Case of Myasthenia Gravis
M3 India Newsdesk Sep 25, 2024
This article delves into the pathophysiology, symptoms, and diagnostic criteria of Myasthenia Gravis. It also emphasises current treatment methods and advancements to improve patient outcomes.
Myasthenia gravis is an autoimmune condition and neuromuscular disease causing skeletal muscle weakness. It works on the muscles in the arms, legs, neck, face, and eyes. Muscle weakness increases with physical activity and decreases following rest. There are antibodies against the acetylcholine receptor, Ach R, in this chronic neuromuscular illness, which results in muscle weakening.
The name “myasthenia gravis” which in Latin and Greek in origin means” grave, or serious muscle weakness. With the treatment available, disease symptoms are controlled and patients have a better quality of life and life expectancy.
Types of myasthenia gravis
1. Autoimmune
- Ocular
- Generalised
2. Congenital
3. Neonatal
Symptoms Onset may be sudden:
- Muscle weakness
- Fatigue
- Droopy eyelids
- Blurred or double vision
- Difficulty speaking
- Swallowing or chewing
- Limited facial expression trouble walking
- Shortness of breath
- Weakness in arms, hands, fingers, legs and neck
Myasthenia gravis patients who have severe weakness may experience respiratory failure and need emergency medical attention right away.
Case description
- A 34-year-old male comes with complaints of sudden onset left-sided ptosis for 10 days, there is occasional diplopia on certain gaze.
- No f/o facial weakness, dysphagia, limb weakness, dysarthria, loss of consciousness or seizures, and No breathing difficulties.
- The patient complained to an ophthalmologist about rapid changes in facial look and double vision.
- There is occasional diplopia on certain gazes.
- No f/o facial weakness, dysphagia, limb weakness, dysphagia, loss of consciousness or seizures.
- He was directed to a neurologist and urged to get an MRI Brain provided eye drops.

Fig.1 Early Pic. Of the pt. when no symptoms

Fig.2 when pt started having symptoms.
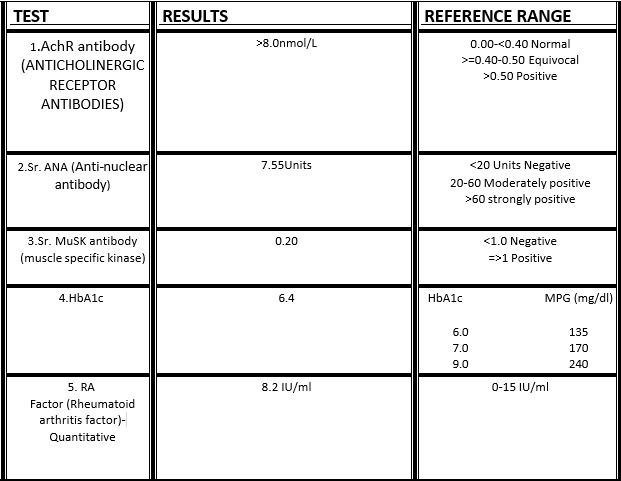
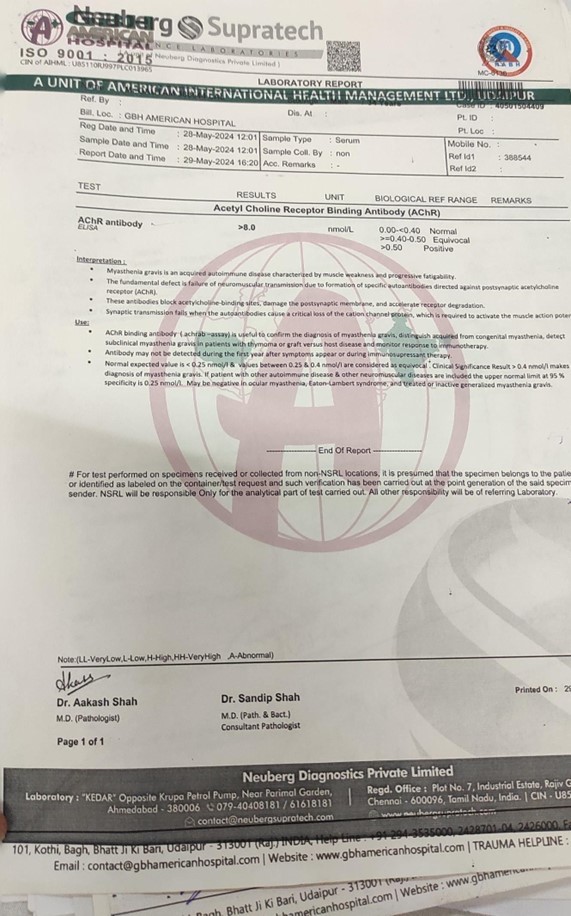
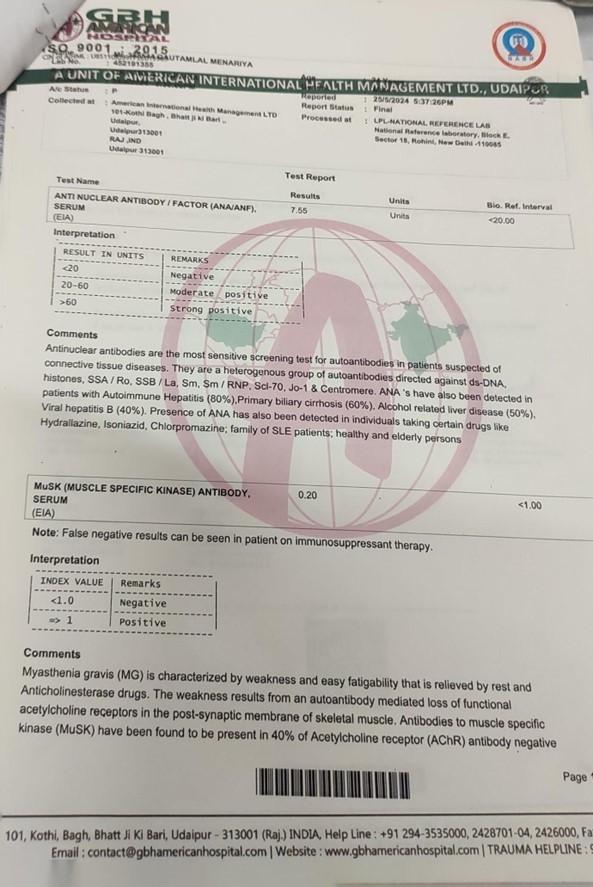
The patient has had CAD in the past and is on statins, dual antiplatelets, and anti-angina drugs. On investigations, positive anti AchR ab was found ( >8 nmol/Lt. normal >0.50).
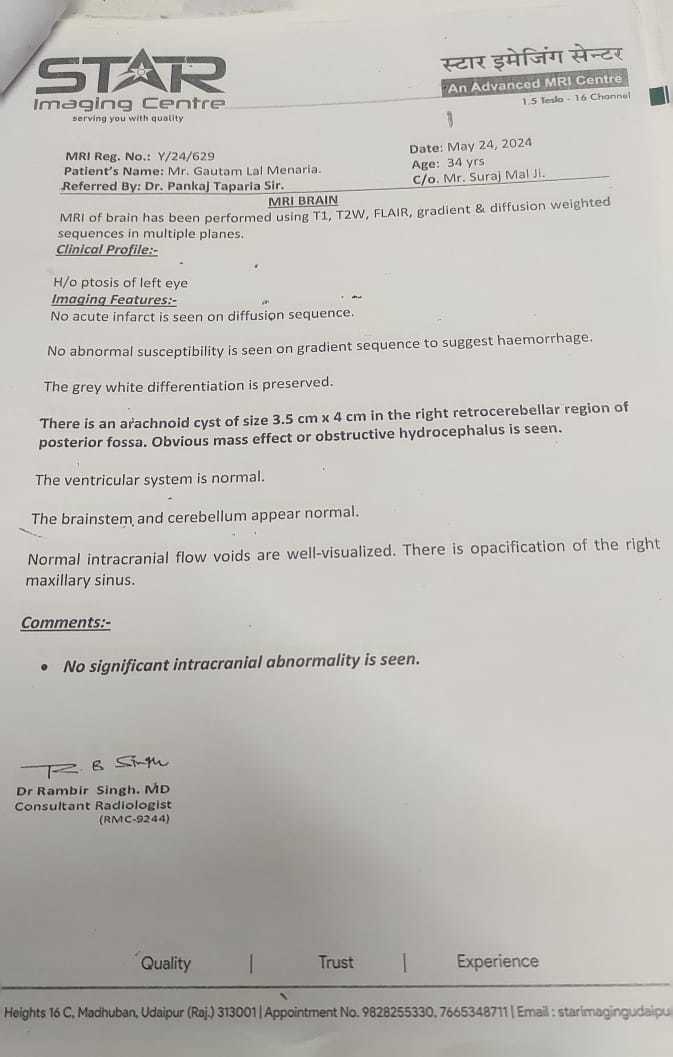
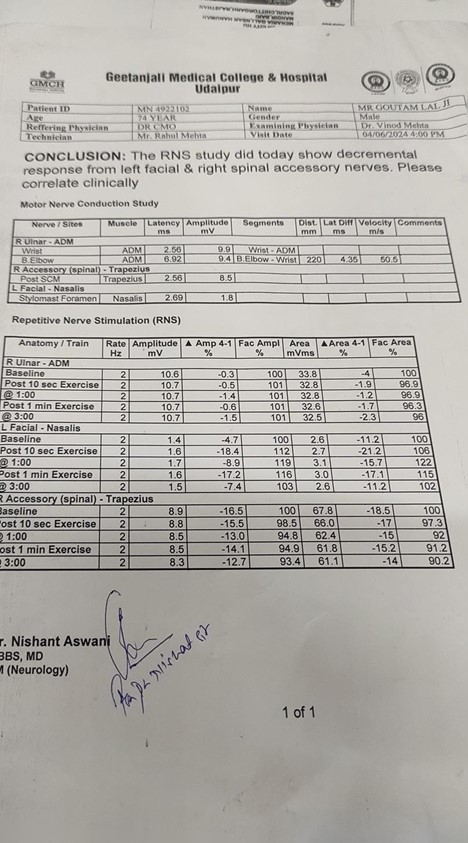
MRI BRAIN s/o arachnoid cyst 3.5 ×4 cm in Rt retro cerebellar region in the posterior fossa.obvious mass effects /obstructive hydrocephalus. RNS s/o decremental response from left facial and right spinal accessory nerves.
Treatment
- The patient was treated with T Distinone 60mg QID, T Azoran BD, and T Omnacortil.
- The patient replied at first, but he was unable to fully recover, and a few days later, he began to experience difficulty swallowing and speaking.
- After receiving IV immunoglobulin therapy for two sessions, the patient began to improve and recuperate. He was admitted to the hospital right away.

Fig. 3 Pt in Recovering state after receiving IV Immunoglobulin
- The above patient is on T. Distinone 60mg tds, T. Azoran50mg OD and doing well on regular follow-up.
What is the myasthenia crisis?
It Is a medical emergency that occurs when the muscles that control breathing weaken to the point where individuals require a ventilator. It could be brought on by an infection, stress, surgery, or a drug side effect.In people with myasthenia gravis, between 15% to 20% go through at least one myasthenia crisis. However, the myasthenia crisis in up to 50% of cases may have no apparent explanation.
What causes myasthenia gravis?
- Being an autoimmune disease, myasthenia gravis causes the immune system—which ordinarily defends the body against external substances—to inadvertently target itself.
- In Myasthenia, antibodies (immune proteins produced by the body’s immune system) block, alter, or destroy the receptors for acetylcholine at the neuromuscular junctions, which prevents the muscle from contracting. This is most often caused by antibodies to the acetylcholine receptor itself, but antibodies to other proteins, such as MuSK (Muscle-specific kinase ) protein, also can repair the neuromuscular junction.
- Men and women of diverse cultural and racial origins can get myasthenia gravis. It is most common in young adult women (under 40) and older men (over 60), but it can occur at any age, including during childhood. Myasthenia gravis is not inherited nor it is contagious. On rare occasions, multiple family members may experience the condition.
- Neonatal myasthenia, a syndrome where a mother with myasthenia gravis acquires antibodies from her fetus, is an uncommon manifestation of myasthenia gravis.
- Neonatal myasthenia is generally temporary, and the baby’s symptoms usually disappear within 2-3 months after birth. Congenital myasthenia is a rare condition that can occur in healthy mothers' infants. It is not an autoimmune disorder; instead, it is brought on by faulty genes that result in aberrant proteins in the neuromuscular junction, which can mimic the symptoms of myasthenia gravis.
How is myasthenia gravis diagnosed?
Clinically, by Symptomatology and neurological examination, assessing muscle strength, tone, coordination, sense of touch, and look for impairment of eye movements.
2. Edrophonium test
Use of inj. Edrophonium chloride briefly relieves weakness in myasthenia gravis people, the medication blocks the breakdown of acetylcholine & temporarily increases the levels of acetylcholine at the neuromuscular junction, also used to test ocular muscle weakness.
3. Blood test
Acetylcholine receptor antibody levels are abnormally increased in the majority of myasthenia gravis patients. A second antibody called the anti-MuSK antibody has been found in about half of individuals with myasthenia gravis who do not have acetylcholine receptor antibodies, a blood test can also detect this antibody, however in some individuals with myasthenia gravis, neither of these antibodies is present, hence called seronegative myasthenia.
4. Electrodiagnostics
- Repetitive nerve stimulation is a diagnostic technique that involves repeatedly stimulating a person's nerves with tiny electrical pulses to exhaust particular muscles.
- Musclefibres in myasthenia gravis, as well as other neuromuscular disorders, do not respond as well to repeated electrical stimulation compared to muscles from normal individuals.
- Single fibre electromyography (EMG), considered the most sensitive test for myasthenia gravis, detects impaired nerve-to-muscle transmission.
- When other tests fail to show abnormalities, electromyography (EMG) can be very helpful in detecting mild cases of myasthenia gravis.
5. Diagnostic imaging
Diagnostic imaging of the chest using computed tomography (CT) or Magnetic resonance Imaging (MRI) may identify the presence of thymoma.
6. Pulmonary function imaging
It is possible to forecast whether respiration will fail and result in a myasthenic crisis by measuring breathing strength.
Treatment of Myasthenia Gravis
1. Thymectomy
The removal of the thymus gland helps to rebalance the immune system and reduces muscle weakness and the need for immunosuppressive medicines.
2. Monoclonal antibody
In 2017, the US FDA approved the use of eculizumab for the treatment of generalised myasthenia gravisin adults who test positive for the anti-acetylcholine receptor antibody.
3. Anticholinesterase medications
Pyridostigmine is used to promote neuromuscular transmission and build muscle strength by slowing down the breakdown of acetylcholine at the neuromuscular junction.
4. Immunosuppressive drugs
The medications—prednisolone, azathioprine, mycophenolate mofetil, and tacrolimus—increase muscle strength by inhibiting the synthesis of aberrant antibodies. FDA has approved 2 drugs for myasthenia gravis, rystiggo (rozanolixizumab noli) and zilbrysa (zilucoplan).
5 Plasmapheresis & intravenous immunoglobulin
Treatment for severe myasthenia gravis focuses on removing damaging antibodies, however, these antibodies only have a short-term effect—a few weeks to months.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Kirti Benal is a Divisional Medical Officer in Railway Hospital, North West Railways, Udaipur
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries