Managing fungal infections in diabetes: Dr Kiran Godse & Dr. Dakshata Tare
M3 India Newsdesk Dec 18, 2018
Dr. Kiran Godse, a noted Dermatologist, and Dr. Dakshata Tare, a senior Dermatologist, share their expertise to help understand the management of dermatophytosis in diabetes mellitus patients, taking into considerations the comorbidities and potential drug interactions due to polypharmacy.

Dermatophytosis is a raging epidemic in India with a paradigm shift in its clinical-epidemiology over the years. The disease has undergone a drastic change in its clinical pattern with frequent recurrences and recalcitrant nature of the infection. Although Trichophyton rubrum is the most common organism in India, many recent Indian studies have found Trichophyton mentagrophytes and Microsporum audonii to be the dominant pathogens.
These are responsible for the inflammatory lesions of tinea. Besides, the host factors such as increasing urbanisation, overcrowding, poverty, non-compliance, the rampant use of irrational fixed drug combinations available as ‘over the counter’ products that contain a steroid, antifungals and antibacterials have led to the emergence of steroid-modified tinea (tinea incognito) which is also resistant to antifungals.
Local T cell-mediated immunity is essential to curb the spread of fungal infection. The inflammatory response mounted by the body limits the spread of tinea. However, the suppressed host immunity leads to ineffective elimination of the fungus making the disease more chronic and extensive.
Various reports mention a rise erythrodermic tinea, Trichophyton rubrum related tinea corporis generalisation and multiple site involvement. In addition, atypical lesions such as multiple irregularly shaped lesions, eczematous change in the centre, extensive tinea faciei, male genital involvement, ‘ring- within-a- ring’ appearance known as tinea pseudoimbricata, lesions with pustular borders are being commonly encountered.
The standard treatment regimens used earlier are no longer effective and more aggressive management is needed to bring a clinical cure. Even in limited involvement, the presence of comorbidities is an indication for systemic drugs.
Diabetes and polypharmacy
Diabetes mellitus is a state of suppressed immunity predisposing to increased risk of fungal infections particularly tinea pedis, onychomycosis and candidiasis as mentioned earlier. The patients also suffer from a host of other comorbidities like hypertension, dyslipidemia and coronary heart diseases. Comorbidities essentially lead to polypharmacy and many of these drugs have significant clinical drug interactions with antifungal agents. Hence, when treating fungal infections in diabetics, these drug interactions need to be taken into consideration.
Systemic antifungals
The five main agents available are
- Itraconazole
- Fluconazole
- Terbinafine
- Griseofulvin
- Ketoconazole
A new generation of systemic antifungals has been developed including posaconazole and voriconazole and ravuconazole.
Azole antifungals
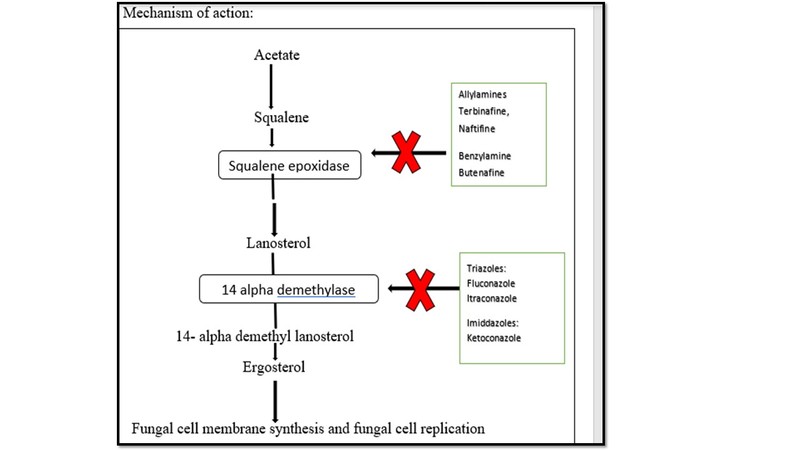
Azoles are fungicidal drugs that inhibit lanosterol demethylase. This leads to the accumulation of abnormal sterols and defective cell wall and ultimately fungal death.
- Itraconazole
Since diabetic patients present with polypharmacy, to avoid potential drug interactions itraconazole should be avoided.
Dosage: [5mg/kg] 200-400 mg o.d. × 4-6 weeks;
For Onychomycosis:
- Continuous: Fingernail 200 mg o.d. × 2 months; Toenail 200 mg o.d. × 3 months;
- Pulse therapy: Fingernail 400 mg o.d. × 7 days, for 3-4 months; Toenail 400 mg o.d. × 7 days, for 3-6 months
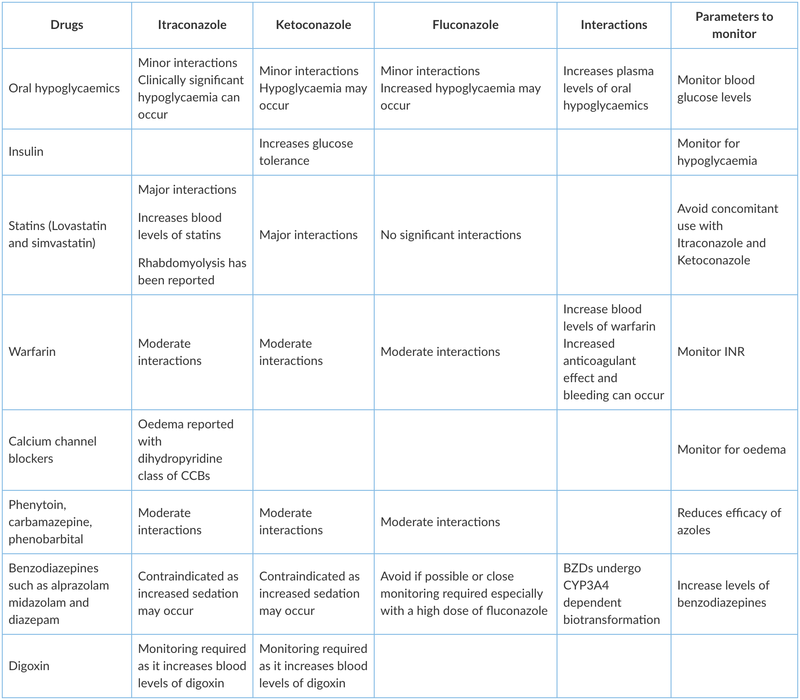
Itraconazole is metabolised by the cytochrome P450 3A4 enzyme pathway. Oral hypoglycaemic medications such as sulphonylureas are also metabolised by this pathway increasing the potential drug interactions. These drugs include tolbutamide, glibenclamide and glipizide. Itraconazole can increase the plasma levels of these drugs, resulting in hypoglycemia. Itraconazole also interacts with HMG-CoA reductase inhibitors(statins), calcium channel blockers, warfarin, anti-arrhythmic drugs and benzodiazepines.
Itraconazole is a lipophilic and keratophilic triazole. It is more specific for fungal cytochrome P450 than ketoconazole resulting in less toxicity and more efficacy than the latter. The drug is well absorbed, and absorption is better when taken with food. It reaches stratum corneum through sweat, sebum and incorporation into the basal layer. It readily penetrates the nail via the nail bed and matrix. It does not get redistributed in the circulation and measurable drug levels are seen in stratum corneum for 3-4 weeks after discontinuation of therapy. It has a broad spectrum of antimicrobial action and is effective against dermatophytes as well as molds and yeasts.
- Ketoconazole
It also has significant drug interactions with other drugs and hence should not be used in diabetics.
It was the first oral imidazole available for the treatment of mycotic infections. Its use has been supplanted by other antifungals as hepatitis is an important dose-related side effect seen with ketoconazole.
- Fluconazole
For DM patients, Dose adjustment may be required according to creatinine clearance.
Dosage: [3-6mg/kg] ; 150-300 mg × once/week for 4-6 weeks
For onychomycosis: Fingernail: 150-300mg/ week for 3-6 months;Toenail 150-300 mg/week for 6-12 month
It is a triazole with high water solubility and is well absorbed through the oral route. It can be given as single dose regimes as it has a long half-life. It is excreted through the renal route and hence dose adjustment is required according to creatinine clearance. Its interaction with other drugs is mentioned in the table.
Allylamines
- Terbinafine
Thus terbinafine is relatively safer and more effective option than azoles in DM, despite having reduced efficacy against yeasts.It has a reduced risk of interaction with insulin and/or oral hypoglycemic medications as it metabolises via cytochrome P450 2D6 enzyme. It has significant interaction with a host of other drugs like beta blockers, tricyclic antidepressants, antiarrhythmic drugs. Since polypharmacy is common in DM, it should be prescribed with caution in diabetics.
Dosage: [ 250mg/day for > 40kg, 125 mg/kg for 20-40 kg and 62.5 mg/kg for < 20kg body weight]
Terbinafine: 250 mg o.d. × 4-6 weeks; For onychomycosis: Fingernail 250 mg o.d. × > 6 weeks ;Toenail 250 mg o.d. × 12 weeks
It inhibits squalene epoxidase leading to accumulation of intracellular squalene and deficient ergosterol, resulting in fungal cell death. The drug is well absorbed orally and reaches skin through two paths: diffusion from the vessels through the dermis or epidermis and via sebum in the hair follicle and skin.
- Griseofulvin
It can be safely used in diabetics.
Dosage: [15-25 mg/kg bod weight] 500 o.d. × 4-8 weeks; For onychomycosis: Fingernail 500 mg o.d. × > 6 months; Toenail 500 mg o.d. × > 12 months
It is a fungistatic drug. It inhibits the formation of microtubules thus inhibiting the fungal cell division. Absorption significantly increases with fatty meals. Phenobarbitone reduces the blood levels of griseofulvin. The anticoagulant effect of warfarin is reduced. Griseofulvin is known to cause phototoxicity hence concomitant administration of tetracyclines, sulphonamides and quinolone group of antibiotics should be avoided. It can be safely used in diabetics.
The clinically significant drug interactions of the azole group have been described below.
Topical antifungal agents
Topical antifungals predominantly belong to the group of azoles including triazoles and allylamines. Amorolfine and ciclopirox lacquers are commonly used for onychomycosis.
| Antifungal Class | Examples | Formulations with concentration, with reported frequency of application |
| ANTIBIOTICS | ||
| Polyenes | Amphotericin B | 0.1% liposomal cream: 2 weeks |
| AZOLES | ||
| Imidazoles | Clotrimazole | 1% cream/lotion twice daily: 4 to 6 weeks |
| Ketoconazole | 2% cream/gel once daily: 2 to 4 weeks (shampoo available) | |
| Econazole | 1% cream twice daily: 2 to 4 weeks | |
| Miconazole | 2% cream/gel twice daily: 4 to 6 weeks | |
| Bifonazole | 1% cream once daily: 4 weeks | |
| Oxiconazole | 1% cream/lotion once daily: 4 to 6 weeks | |
| Tioconazole | 1% cream twice daily: 4 weeks | |
| Sertaconazole | 2% cream twice daily: 4 weeks | |
| Luliconazole | 1% cream once daily: 1 to 4 weeks | |
| Eberconazole | 1% cream twice daily: 2 to 4 weeks | |
| Sulconazole | 1% once daily or twice daily: 3 weeks | |
| Fenticonazole | 2% cream twice daily: 4 weeks | |
| Triazoles | Fluconazole | 0.5% gel twice daily: 4 weeks |
| Efinaconazole | 10% nail solution once daily: 48 weeks for toenail onychomycosis | |
| Allylamines | Terbinafine |
1% cream once daily Spray also available: 1 to 2 weeks |
| Naftifine | 1% cream twice daily: 4 weeks | |
| Benzylamines | Butenafine | 1% cream twice daily: 2 weeks (4 weeks for tinea pedis) |
| Morpholines | Amorolfine |
5% nail lacquer once/twice a week for 6 to 12 months 0.25% cream once daily for 4 to 6 weeks |
| Hydroxypyridinones | Ciclopirox 8% |
Nail Lacquer 1% cream once/twice daily for up to 48 weeks Shampoo available |
| Others | Tolnaftate | 1% cream/lotion twice daily: 4 weeks |
| Oxaboroles | Tavaborole 5% | Nail solution once daily for 48 weeks |
| Nonspecific agents | Whitfield's ointment Castellani's (carbol-fuchsin) paint |
Note: Duration of treatment varies according to the site. Tinea pedis requires a longer duration (at least 4 weeks) in comparison to tinea corporis.
Mechanism of antifungal action
| Azoles |
|
| Allylamines |
|
| Ciclopirox |
|
| Amorolfine |
|
Other actions of Antifungals
- Anti-inflammatory action
- Azoles like sertaconazole, econazole, clotrimazole, miconazole exert anti-inflammatory action. They inhibit the release of interferon alpha, interleukin 2 (IL-2), IL-4 and granulocyte- macrophage-colony-stimulating factor from activated lymphocytes. Clotrimazole, Miconazole also inhibit the chemotactic ability of polymorphonuclear leukocytes.
- Allylamines exert an inhibitory action on chemotaxis of polymorphonuclear cells and reduce the production of reactive oxygen intermediates.
- Anti-bacterial action
- Azoles such as clotrimazole, econazole, miconazole, sertaconazole and allylamines such as terbinafine have anti-bacterial activity against gram-positive bacteria and few gram-negative bacteria.
Studies have reported allylamines to be more effective than azoles due to their faster action and shorter duration of treatment. Luliconazole has better compliance as it is effective on once daily application. As amorolfine has a different mechanism of action than azoles and allylamines, an incidence of resistance to amorolfine is very less and hence should be the treatment choice in recalcitrant infections.
Instructions to enhance the efficacy of topical antifungal therapy
Selection of formulation
Depends on the site of involvement:
- Creams for scaly lesions and glabrous areas
- Lotions on hairy areas, intertriginous areas, extensive areas, weeping lesions
- Lacquers for onychomycosis
- Gels on the face for better cosmetic effect
Frequency of application
- Most topical agents should be applied twice daily except luliconazole which is effective on once daily application
- Topical agents should be applied to the affected area with 2 cm of peripheral normal skin starting from outside to inside
Onychomycosis
- Lacquers should be applied on the nail plate including the nail surface when it is free from the nail bed.
Thus, in DM tinea pedis and onychomycosis are commonly seen which also predisposes to complications like foot ulceration, cellulitis etc. Dermatophytosis needs to be treated aggressively. However, special caution should be taken while prescribing oral antifungals to diabetic patients as polypharmacy is common and antifungals have significant drug interaction profiles.
Read about the identification of common skin infections in Diabetics in the previous part, Identifying common fungal infections in Diabetes Mellitus: Dr. Kiran Godse & Dr. Dakshata Tare
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries