Exclusive series: Diagnosis of Dermatophytosis- Dr. DG Saple
M3 India Newsdesk Feb 19, 2020
Presentation of dermatophytosis lesions has changed in recent years and since lesions are rapidly evolving, it has become mandatory to prevent misdiagnosis or even overdiagnosis of Tinea. In this article, Dr. DG Saple focuses on the laboratory tests for Tinea which can aid in accurate diagnosis of the infection.
Dermatophytosis or ringworm infection can readily be diagnosed on the basis of history and clinical examination. The distribution of the lesions, mainly in the intertriginous regions along with the appearance of the lesion, viz. dry, annular erythematous plaque, active border and central clearing, would normally guide us in clinching the diagnosis. [1]
However, over the last decade or so, the clinical presentation of Tinea has undergone a drastic change, and we no longer get to witness the usual classical presentations which have been accustomed to for so long. Indiscriminate use of topical steroids has been attributed as one of the leading causes responsible for bringing about this catastrophic change.
As the lesions are evolving, the current situation deems it necessary to adopt measures to ensure the correct diagnosis and treatment. Many a times, the annular lesions of Tinea are often misdiagnosed as Nummular eczema and treated with topical steroids. Similarly, Tinea may often be overdiagnosed, and many important conditions may be missed clinically, such as lupus erythematosus or granuloma annulare.
Hence laboratory diagnosis in today’s times is imperative. The investigations may be as simple as an OPD procedure like Potassium Hydroxide (KOH) mount or may require antifungal culture in certain cases.
Potassium hydroxide (KOH) 10% mount
The procedure involves obtaining skin scrapings from the active border of a lesion using a scalpel blade or a glass slide. The scales are the transferred onto a glass slide, wherein a few drops of KOH 10% are added and the preparation is allowed to stand for 15 to 30 minutes to allow the keratin to dissolve. The well-mounted preparation is then examined under a microscope (40X) which allows visualisation of the fungal hyphae which appear as branching, rod-shaped filaments of uniform width with septa (figure 1).
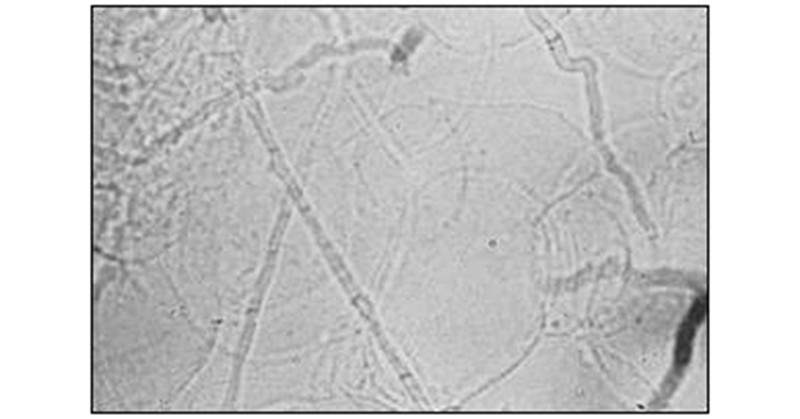
Fig.1: Fungal hyphae
A modification to this method is the use of Chicago Sky-blue stain along with 10% KOH for better visualisation of the fungal hyphae. [2]
Culture
The commonest isolation media for dermatophytosis is Sabouraud dextrose agar (SDA, 4% peptone, 1% glucose, agar, water). The colony develops in about 1 to 2 weeks. Addition of Gentamicin, Chloramphenicol and Cycloheximide is more selective for dermatophytes since Chroramphenicol is inhibitory for saprophytic fungus.
Dermatophyte test medium is an alternative to isolation media that contains addition of pH indicator phenol red. Dermatophytes utilise the protein in the media and turn it from yellow to bright red. [3]
Antifungal Susceptibility & Sensitivity
The standard guideline for anti-fungal drug susceptibility testing for fungi Is CLSI ( Clinical Laboratory Standard Institute) - USA.
- Macro and microdilution method: The minimum inhibitory concentration is defined as the concentration at which the growth of the organism will be inhibited by 80% compared with the growth in the control well.[4]
- Agar dilution method [4]
- Disc diffusion method [4]
- E-strip for determination of minimum inhibitory concentration (MIC). [5]
Histopathology
Hyphae can be seen in the stratum corneum on hematoxylin and eosin staining. Period acid Schiff stains helps to highlight the hyphae.[3]
Dermoscopy
In Tinea corporis, the involvement of vellus hair as seen on dermoscopy is an indicator of systemic therapy. [6]
Polymerase chain reaction and nucleic acid sequence based amplification
It helps in rapid and accurate detection of fungal species and sub-species as well as in determining drug resistance. [7]
However these tests are still in the research stages and require an extensive work-up before they can be made available for day-to-day clinical practice.
This article is part of an exclusive series on Dermatophytosis by Dr. DG Saple. To read the first article, click Emerging recalcitrant dermatophytosis in India
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. DG Saple is a Senior Consultant and Director of Dermatology at a Mumbai-based clinic.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries