The relevance of GABA for diabetes is highlighted in two new studies published in EBioMedicine
Uppsala University News Apr 08, 2018
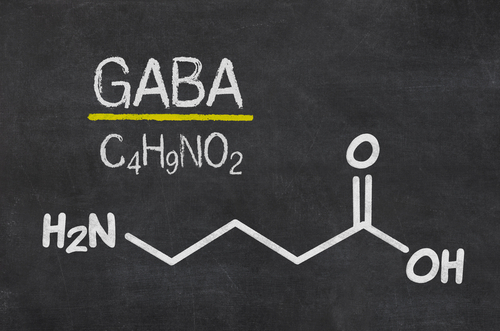
Dynamic interactions between the nervous system, hormones, and the immune system are normally on-going but in diabetes, the balance is disturbed. The two studies published in EBioMedicine by an international research team from Uppsala University highlight the importance of the neurotransmitter beta-aminobutyric acid (GABA) in both type 1 and type 2 diabetes.
GABA is synthesized by an enzyme called GAD from the amino acid glutamate in nerve cells but also, importantly, in the insulin-producing beta cells in pancreatic islets. GAD has two forms, GAD65 and GAD67. In type 1 diabetes, beta cells are destroyed while type 2 diabetes is associated with impaired beta cell function and insulin resistance.
Patients with type 1 diabetes often have antibodies to GAD65. However, there has been no strong link between GABA and type 2 diabetes until recently when it was shown that GABA is important for maintaining and potentially also in the making of new beta cells.
The two current studies, now published in EBioMedicine (http://www.ebiomedicine.com), reinforce the image of GABA's importance, for both types of diabetes. The scientists used ion channels that GABA opens, the GABAA receptors, as a biological sensor for GABA, and were able to determine the effective, physiological GABA concentration levels in human pancreatic islets. They also showed that these ion channels became more sensitive to GABA in type 2 diabetes and that GABA helps regulate insulin secretion (article 1).
The scientists then isolated immune cells from human blood and studied the effects GABA had on these cells. They show that GABA inhibited the cells and reduced the secretion of a large number of inflammatory molecules (article 2).
The anti-inflammatory effect of GABA may be vital in the pancreatic islets since as long as GABA is present, toxic white blood cells can be inhibited, thus increasing the survival of the insulin-secreting beta cells. When the beta cells decrease in number and disappear from the islets as happens in Type 1 diabetes, then GABA consequently is also decreased and, thereby, the GABA protective shielding of the beta cells. When inflammatory molecules increase in strength, it may weaken and even kill the remaining beta cells.
In ongoing studies, the scientists now focus on clarifying the GABA signaling mechanisms in the immune cells and in the human beta cells. They will also study how existing drugs can increase, decrease or mimic the effects of GABA, says Bryndis Birnir.
Articles:
1. Functional characterization of native, high-affinity GABAA receptors in human pancreatic beta cells (2018). Sergiy V. Korol#, Zhe Jin#, Yang Jin, Amol K. Bhandage, Anders Tengholm, Nikhil R. Gandasi, Sebastian Barg, Daniel Espes, Per-Ola Carlsson, Derek Laver, Bryndis Birnir*
2. GABA regulates the release of inflammatory cytokines from peripheral blood mononuclear cells and CD4+ T cells and is immunosuppressive in type 1 diabetes (2018). Amol K. Bhandage, Zhe Jin, Sergiy V. Korol, Qiujin Shen, Yu Pei, Qiaolin Deng, Daniel Espes, Per-Ola Carlsson, Masood Kamali-Moghaddam, Bryndis Birnir*
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries