Initiating Insulin Decisions in Diabetes: Case Study Analysis
M3 India Newsdesk May 02, 2024
Determining when to start insulin therapy in people with diabetes is a problem doctors frequently experience. This article will explore the guidelines and best practices for initiating insulin therapy in diabetes, along with two illustrative case studies.
We are at 100 years of insulin discovery as medical professionals, we often face the challenge of deciding when to initiate insulin therapy in patients with diabetes. This decision requires careful consideration of various factors, including glycemic control, patient preferences, comorbidities, and potential risks and benefits.
Understanding the need for insulin therapy
Millions of people worldwide suffer from diabetes mellitus, a chronic metabolic disease marked by increased blood glucose levels. Despite advances in treatment modalities, some patients with diabetes may eventually require insulin therapy to achieve and maintain optimal glycemic control.
Type 1 diabetes necessitates immediate initiation of insulin therapy due to the absence of endogenous insulin production. In type 2 Diabetes Mellitus, insulin therapy becomes necessary when oral antidiabetic medications, lifestyle modifications, and other non-insulin therapies fail to control blood glucose levels adequately. The decision to initiate insulin therapy should be based on a comprehensive assessment, including the patient's medical history, current treatment regimen, glycemic targets, and individualised care goals.
Guidelines for initiating insulin therapy
The American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) provide recommendations for initiating insulin therapy in patients with diabetes. According to these guidelines, insulin therapy should be considered in the following situations:
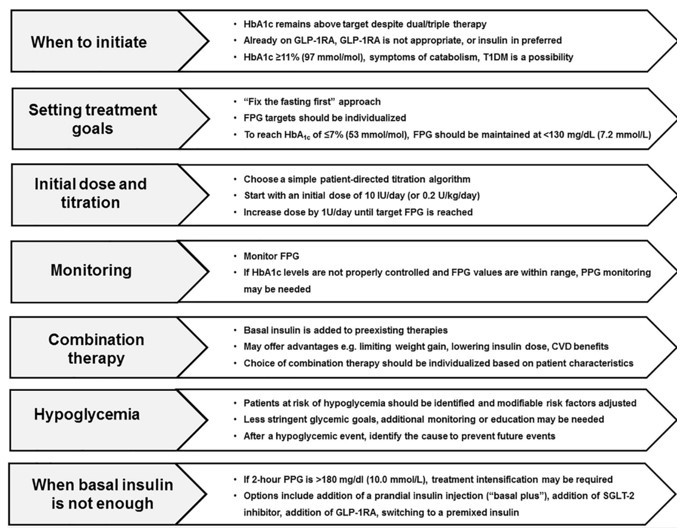
Key considerations when initiating insulin therapy
- Inadequate Glycemic Control: When glycated haemoglobin (HbA1c) levels remain above target despite maximal doses of oral antidiabetic medications or other non-insulin therapies.
- Symptomatic Hyperglycemia: When patients experience symptoms of hyperglycemia, such as frequent urination, excessive thirst, fatigue, or unexplained weight loss.
- Acute Metabolic Decompensation: During acute illness, surgery, or other stressful situations where glycemic control is difficult to achieve with oral medications alone.
- Pregnancy and Gestational Diabetes: Insulin therapy is often required to manage blood glucose levels during pregnancy, especially in women with gestational diabetes.
- Severe Insulin Resistance: In patients with type 2 diabetes who exhibit significant insulin resistance, especially when accompanied by obesity or other metabolic abnormalities.
Case studies
Case study 1
A 52-year-old man was diagnosed with type 2 diabetes eight years ago. Despite multiple oral antidiabetic medications, his glycemic control deteriorated over time, with persistent hyperglycemia and HbA1c levels exceeding 9.0%. He reports frequent episodes of hyperglycemia symptoms, including fatigue and increased thirst. Upon further evaluation, his fasting blood glucose levels consistently exceed 200 mg/dL. Recognising the need for intensified treatment, I engaged the patient in a comprehensive discussion. The patient agrees to start basal insulin therapy in addition to his current oral medications.
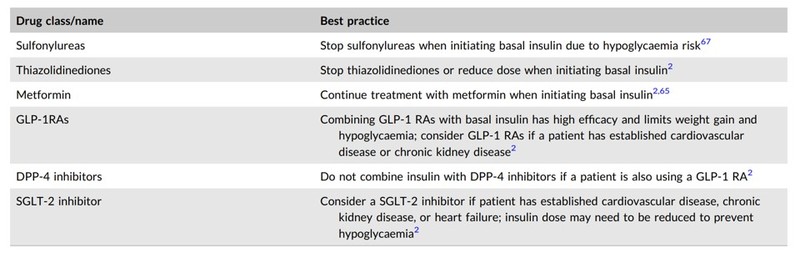 Best practices when combining insulin with non‐insulin anti‐hyperglycemic treatments
Best practices when combining insulin with non‐insulin anti‐hyperglycemic treatments
Factors influencing insulin initiation:
- Disease progression: As diabetes progresses, beta-cell function declines, necessitating exogenous insulin administration to maintain optimal glycemic control.
- Lifestyle modifications: The patient's weight gain over the years led to insulin resistance. Encouraging lifestyle modifications, such as dietary changes and physical activity, remains essential, but its impact may take time to manifest.
- Patient empowerment: Open, honest conversations with patients regarding the progressive nature of diabetes can foster trust and facilitate their acceptance of insulin therapy.
Insulin initiation process:
- Patient education: I ensured that the patient understood the rationale behind initiating insulin therapy, and debunking any myths or misconceptions. Education also involved discussing insulin types, administration techniques, glucose monitoring, and potential side effects.
- Individualised approach: Considering the patient's dietary preferences, lifestyle, and daily routine, we chose basal insulin therapy in addition to his current oral medications. This allowed for flexibility in titrating and matching insulin doses to his carbohydrate intake and glucose levels.
- Safety monitoring: Regular glucose monitoring, frequent clinic visits, and telemedicine support during the initial phase are pivotal for dose adjustments, detecting hypoglycemia, and addressing patient concerns.
Case study 2
A 34-year-old woman with type 1 diabetes, presented with recurrent hypoglycemia and difficulty managing her glucose levels despite multiple daily injections. Recognising her distress, I embarked on finding a solution to improve her quality of life.
Factors influencing insulin initiation:
- Disease type: Type 1 diabetes necessitates immediate initiation of insulin therapy due to the absence of endogenous insulin production.
- Hypoglycemia and glucose variability: Frequent hypoglycemic episodes and erratic glucose fluctuations compromise the patient’s well-being, potentially leading to impaired cognitive functions, anxiety, and reduced quality of life.
- Psychological impact: Living with a chronic illness can take an emotional toll on patients. Addressing mental health concerns associated with diabetes is crucial to ensure successful treatment outcomes.
Insulin initiation process:
- Identification of hypoglycemia triggers: Close monitoring of the patient's glucose levels, dietary patterns, healthcare routines, and exercise regimen helped identify the triggers for her hypoglycemic episodes.
- Adjusting insulin regimen: Transitioning the patient to an insulin pump allowed for precise insulin dose adjustments based on her real-time glucose readings. This method aimed to reduce hypoglycemia while improving overall glycemic control.
- Psychological support: Collaborating with mental health professionals equipped the patient with the tools to address anxiety and emotional distress associated with her condition, ensuring a holistic approach to her treatment.
There are several factors to consider when initiating insulin pump therapy, including the patient's insulin needs and their ability to manage the device. In the case of the patient, her insulin needs appear to be relatively stable, and she has a good understanding of how to manage her diabetes.
The next step is to program the insulin pump to meet the patient's needs. This involves calculating the patient's total daily dose of insulin (TDD) and determining the basal rate of insulin, which is the amount of insulin delivered continuously throughout the day. For the patient, her TDD is calculated to be 60 units, with a basal rate of 1 unit per hour.
Once the insulin pump is programmed, the patient must learn how to use it effectively. This includes learning how to check blood glucose levels and adjust the pump settings as needed. The patient works closely with her healthcare team to ensure that she understands how to use her new insulin pump.
Conclusion
Initiating insulin therapy in patients with diabetes requires a careful assessment of various factors, including glycemic control, patient preferences, comorbidities, and potential risks and benefits. By following evidence-based guidelines and individualising treatment plans, healthcare providers can optimise patient outcomes and improve the quality of life for individuals with diabetes.
Through the presented case studies, we have highlighted the importance of timely initiation of insulin therapy in patients with inadequate glycemic control and symptomatic hyperglycemia. By addressing the unique needs of each patient, we can effectively manage diabetes and reduce the risk of complications associated with uncontrolled hyperglycemia.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Shravan Kumar is a consultant diabetologist from Khammam.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries